New system could provide detailed images—even of soft tissue—from a lightweight, portable device.
X-rays transformed medicine a century ago by providing a noninvasive way to detect internal structures in the body. Still, they have limitations: X-rays cannot image the body’s soft tissues, except with the use of contrast-enhancing agents that must be swallowed or injected, and their resolution is limited.
But a new approach developed by researchers at MIT and Massachusetts General Hospital (MGH) could dramatically change that, enabling the most detailed images ever—including clear views of soft tissue without any need for contrast agents.
Photos of the Day: Contrast-Free Portable X-Rays
The work will be presented by MIT postdoc Shuo Chen at the 13th International Workshop on Micro and Nanotechnology for Power Generation and Energy Conversion Applications (PowerMEMS 2013), being held Dec. 3 to 6 in London.
The new technology “could make X-rays ubiquitous, because of its higher resolution, the fact that the dose would be smaller and the hardware smaller, cheaper, and more capable than current X-rays,” says Luis Velásquez-García, a principal research scientist at MIT’s Microsystems Technology Laboratories and senior author of the PowerMEMS paper.
Velásquez-García says that while conventional X-ray systems show little or no structure in most soft tissues—including all of the body’s major organ systems—the new system would show these in great detail. A test the team performed with an eye from a cadaver using X-rays from a particle accelerator clearly shows “all the structures, the lens and the cornea,” he says. “In time we are confident our system will be able to achieve such resolution with a far simpler and cheaper device.”
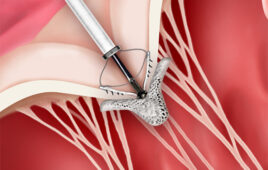
The key is to produce coherent beams of X-rays from an array of micron-sized point sources, instead of a spread from a single, large point as in conventional systems, Velásquez-García explains. The team’s approach includes developing hardware that is an innovative application of batch microfabrication processes used to make microchips for computers and electronic devices.
Using these methods—alternating between depositing layers of material and selectively etching the material away—the MIT researchers have produced a nanostructured surface with an array of tiny tips, each of which can emit a beam of electrons. These, in turn, pass through a microstructured plate that emits a beam of X-rays.
Using the first version of the cathode, the team was able to capture high-resolution absorption images of samples where fine soft-tissue structures are clearly visible. “This is very exciting,” Velásquez-García says. “We just started, but we are confident we are on the right path.”
The resulting coherent beam of X-rays from the optimized cathode chip would be equivalent to something that can now be produced only by “incredibly expensive” systems at linear particle accelerators, Velásquez-García says. But those facilities have demonstrated the diagnostic power of the images they can produce—for example, clearly revealing the presence of a cancerous tumor by showing the details of the blood vessels supplying it. Similarly, an image of a knee reveals all the ligaments, muscle attachments, and fine details of the bone structures that cannot be seen at all on conventional X-rays.
“You can’t have a linear accelerator in every hospital,” Velásquez-García says. But the new system could potentially improve the resolution of X-ray imagery by a factor of 100 with hardware that costs orders of magnitude less, he says.
Even when soft tissue can be imaged conventionally by adding contrast agents such as barium, the use of those agents takes extra time, and the agents themselves can pose risks, he says. And because the new system is electronic—today’s thermionic systems take time to heat up—it can be switched on and off much faster, resulting in a much lower dose of radiation to the patient, Velásquez-García says.
He says the technology could also have applications beyond the medical field. For example, X-rays are used to check for defects in composite materials; the portability of the new system could allow more widespread use of such safety measures. The new system could also be useful in airport screening of baggage, where its ability to distinguish among liquids could make it much easier for agents to differentiate a harmless bottle of shampoo from a container of explosive material or a hazardous chemical.
The test device the team built, working with Rajiv Gupta of MGH, is housed in an 8-inch metal cube, about the size of a shoebox. The team expects to spend two to three years refining and improving the design, Velásquez-García says; commercial versions could be available within a few years after that.
Christopher Holland, a principal scientist at Micro Science Engineering Laboratories in Menlo Park, Calif., who was not involved in this work, says, “The approach being pursued by the authors of this article and others on the MIT team is novel and has significant potential for imaging soft tissue using X-rays.” He cautions, “The demonstration in this paper is only a laboratory demonstration and not yet portable,” but says it is “a steppingstone on that path.”
The research, which also included MIT postdoc Frances Hill and graduate student Eric Heubel, was funded by the Defense Advanced Research Projects Agency.