Patients who trained throughout 2014 with the WAP’s brain-controlled system regained the ability to voluntarily move their leg muscles and to feel touch and pain in their paralyzed limbs.
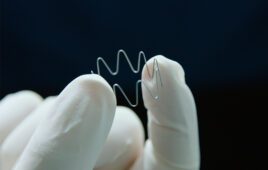
During the 2014 FIFA World Cup opening ceremony, a young Brazilian man, paralyzed from the chest down, delivered the opening kickoff. He used a brain-machine interface, allowing him to control the movements of a lower-limb robotic exoskeleton.
This unprecedented scientific demonstration was the work of the Walk Again Project (WAP), a nonprofit, international research consortium that includes Alan Rudolph, VP for research at Colorado State University, who is also an adjunct faculty member at Duke University’s Center for Neuroengineering.
Barely two years after the demonstration, the WAP has released its first clinical report, published Aug. 11, 2016, in Scientific Reports. A group of patients who trained throughout 2014 with the WAP’s brain-controlled system, including a motorized exoskeleton, regained the ability to voluntarily move their leg muscles and to feel touch and pain in their paralyzed limbs. This, despite being originally diagnosed as having a clinically complete spinal cord injury – in some cases more than a decade earlier.
The patients also regained degrees of bladder and bowel control, and improved cardiovascular function, which in one case resulted in a reduction in hypertension. This is the first study to report that long-term brain-machine interface use could lead to significant recovery of neurological function in patients suffering from severe spinal cord injuries.
The WAP researchers theorize that the long-term training regimen likely promoted brain reorganization and activated dormant nerves that may have survived the original spinal injury from 3 to 14 years earlier.
The researchers, led by neuroscientist Miguel Nicolelis, director of the Duke University Center for Neuroengineering and president of the Alberto Santos Dumont Association for Research Support, say they don’t yet know the limits of this clinical recovery as patients have continued to improve since the World Cup demo. However, they believe their initial findings could influence future clinical practices for paraplegic patients by upgrading brain-machine interfaces from a simple assistive technology to a potential new therapy for spinal cord injury rehabilitation.
Paper co-author Rudolph joined the WAP team prior to coming to CSU in 2013. A former program manager at DARPA, Rudolph led a brain-machine interface research effort starting in 1998 that helped the Duke neuroengineers develop pre-clinical demonstrations. These efforts led to the human clinical trials in the WAP.
Rudolph also started a nonprofit foundation, the International Neuroscience Network Foundation, that works closely with AASDAP, which supports the WAP. Rudolph was recruited by Nicolelis in 2011 to manage the WAP, leading the transdisciplinary, international group of 100 scientists in communication and meeting deadlines. Rudolph also connected the project with CSU’s Idea-2-Product 3D printing lab, which custom-printed the liner of a helmet worn by the paraplegic patients.
Rudolph is passionate not only about the technological advances the new brain-machine interface represents, but also what it could mean for paralyzed patients.
“This has been a tremendous journey, to start working on this phenomenal project over 15 years ago on ideas first demonstrated in animals, and that are now showing revolutionary theories of how the brain works,” Rudolph said. “The WAP scientists are making real impact in helping impaired people walk again. Seeing faces of young adults walking for the first time in many years has been life-changing for all of us.”
Rudolph has continued advocating strongly for the WAP project and for brain-machine interface science in general, at CSU and elsewhere. Last June, Rudolph also organized for a delegation from Colorado Gov. John Hickenlooper’s office to visit WAP scientists in Brazil.
Next steps
Nearly all of the patients described in the study have continued their rehabilitation, now exceeding two years of training, Nicolelis said. He and colleagues plan to publish additional data about participants’ continued progress. They also plan to create a new trial with patients who suffered more recent spinal cord injuries to see whether quicker treatment can lead to faster or better results.
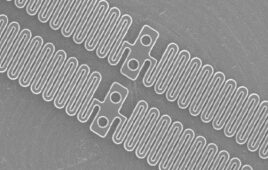
The team also continues efforts to adapt technologies that are accessible for patients around the world who don’t have access to physical therapy centers with the latest equipment. Perhaps the best answer is haptic sleeves, which by comparison are affordable and something a patient could use at home, Nicolelis said.
Until now, no clinical study employing brain-machine interfaces in patients suffering severe spinal cord injuries reported any neurological improvements. Nicolelis believes this was due to the short-term nature of those studies, which usually involved only one human subject. In addition, none of these studies included detailed neurological evaluations to search for clinical improvement.
Colorado State University
colostate.edu
Duke University
duke.edu