(Credit: Thomas Jull)
There’s no doubt that over the past few years the cost of healthcare has risen significantly.
This situation is leaving many patients with an empty wallet and putting them under pressure to come up with ridiculously large, ongoing funds in order to stay well (and in some cases even stay alive) through continued treatment.
Recent stories in the spotlight include the EpiPen price hike which has seen some brands increase their consumer ticket more than 500% since 2008, from $100 to over $600 for a two-pack. And then there was the price rise for the drug Daraprim back in 2015, where retail spiked from $13.50 a tablet to $750 ‘overnight’.
Although Big Pharma business strategies are not the only contributors to the increases in health care costs, they do fit the trend – According to a report from CNBC back in May 2016, the cost of healthcare for the average family in the U.S. is now over $25K per year, triple that of 2001.
So, we ask the question, can medical devices provide the ‘hack’ to tackle healthcare expenditure head-on?
Reducing labor costs involved with treating disorders
If we look at the clinical setting over the past 15 years, it is clear that Point-of-Care Testing (POCT) and associated technology has significantly reduced the amount of manual labor involved in diagnosing disorders at the time of test. Similarly, these affordances have reduced the time it takes to obtain results.
This shift, from analyzing the test sample in a lab away from the clinic to analyzing it on the bench within the clinic (or at the bedside in the hospital), has been a major factor in providing leaner workflow; by eliminating the lab technician’s role and/or other supporting medical staff, you minimize labor while obtaining the same result.
However, research into the costs of POCT versus the central laboratory test suggests that in some cases there is no economic savings to be had from the former method. A study from Lewandrowski & Lewandrowski in 2013 found that POCT actually added $4.74 per test compared to central lab testing for whole blood creatinine.
Despite this, through simpler design, ease of use and increased onboard capabilities, permitted by technology advancement, medical devices for treating disorders are reducing labor associated with medical staff involvement. Not only are devices shortening the length of treatment time but they are also replacing the higher compensated operator, once the doctor, with a nurse or even the patient themselves.
A good example of this is the use of blood glucose monitoring systems for patients who have diabetes.
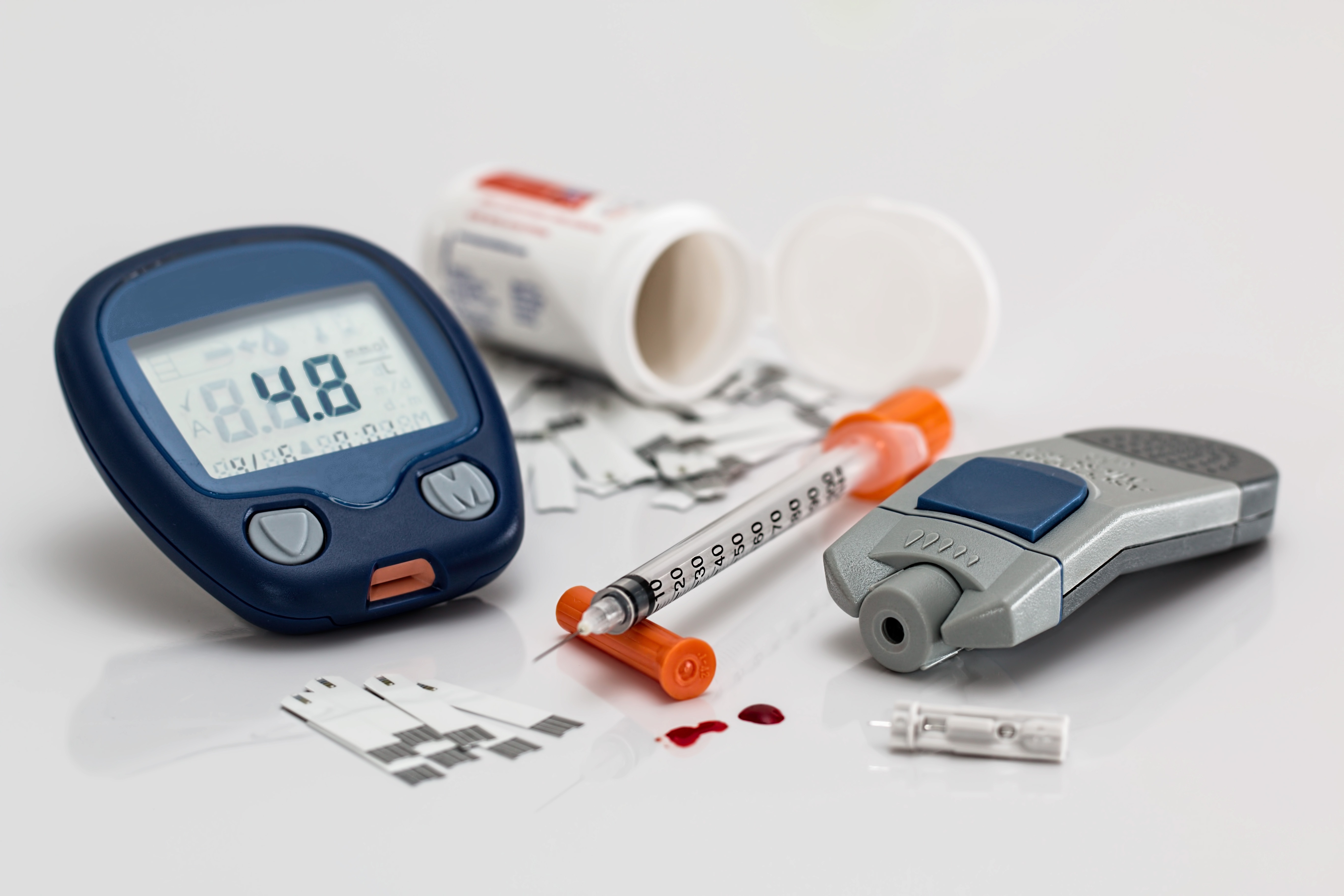
(Credit: Thomas Jul)
The FreeStyle Optium Neo from Abbott Diabetes Care can help with the management of the condition – once set up by a health care provider, the device can be used for logging, displaying, and suggesting insulin dose adjustments. As the device is able to guide patients through their treatment, it saves them and the clinic/hospital costs associated with staff labor. [Source: Newmarker, 2014]
Medical Devices like this enable patients to integrate treatment seamlessly into their lives, so as well as saving time and money it gives the patient themselves control over their condition.
Moving treatment from the clinical setting to the home
It’s widely agreed that the next step away from large costs associated with the clinical setting is to move healthcare out of the hospital and into the patient’s home, or onto their person.
Technologies, such as telehealth and data collection via mobile apps, are leading the way in this shift, by enabling home-based monitoring and therapies. Importantly, these technologies are also leveraging the intelligence available in consumer electronic devices.
To put things into perspective, the average U.S. hospital stay is nearing $2000 per night, and if you get there by ambulance you’ll pay around an extra $1000 taxi fare. Although there are costs associated with home-based monitoring and therapies, such as additional/specialized equipment and in some cases house visits, ‘room and board’ is already paid for upfront by the patient (it’s their home!). Not only does this provide value in cost savings but it also provides value to the patient via comfort, minimal disruption and ease of treatment.
When it comes to being able to treat conditions with the technology already available in consumer electronics (which most patients already own and are familiar with using) the cost savings are even greater compared to conventional clinical treatment or monitoring.
Utilizing technology in smartphones helps medical device companies reduce their development costs dramatically as they can make use of the products existing hardware – the phones camera flash can be a device’s excitation light source, the camera itself can be the emission detector (with lenses), the touchscreen provides the user interface for control input and viewing of results, the processor is used to control and run the algorithm and software/app, Bluetooth and wireless used for communications and for uploading/downloading to other devices, the rechargeable battery provides the power source and mobility, and its all packaged in a stylish casework courtesy of Steve Jobs’ design team.
To develop and package such technology from scratch would cost millions of dollars, so it’s no wonder that the number of health and medical apps available had doubled in September 2015 from two years previously. [Source: Misra, 2015]
In addition, wearables are also a growing technology helping to move ‘treatment’ out of the clinic and thus reducing healthcare costs. The effectiveness of wearables in providing a healthcare solution is still debated by industry voices, but I personally see them as an investment in an individual’s health and an opportunity for MedTech innovators – see my latest MDT blog on wearables.
Managing chronic problems more effectively
In essence, the very act of performing healthcare at home or via wearables can be seen as managing problems more effectively. As well as saving costs by keeping people out of hospital, these new methods bring with them further benefits in the way of care.
Evidence shows that devices are finding ways to provide cost savings at the same time as managing problems more effectively compared to medication.
For those living with atrial fibrillation, which can lead to a stroke, the Watchman device from Boston Scientific provides an alternative solution to blood-thinning medications such as Warfarin and NOAC’s.
Amazingly, research performed on the effectiveness and cost of this device, something which is implanted into the heart to close off the left atrial appendage, has found that it is more effective and less costly to Warfarin at 10 years and dominant to NOACs at five years, with cost savings generated annually thereafter [Source: Diagnostic and Intervention Cardiology, 2016].
This is a great example of a medical device replacing a patient’s prescription of life long medication for a specific condition.
Reducing costs upstream through less expensive device manufacture
It’s not surprising that cutting costs upstream during device manufacture can help reduce downstream expenses of healthcare passed onto the patient later on.
This brings us onto examine reimbursement, which, when it comes to device manufacturers can be a major driving force in device design.
The healthcare payment system in the US, consisting of a fee-for-service model, paid by third party (insurance companies) and public payers (Medicare), requires manufacturers to consider the cost of production early on.
Naturally, the traditional techniques of cheaper price per part through production of higher volume, removal of waste through lean processes, and efficient supply chain management still largely influence the bottom line cost savings for devices.
However, devices are becoming less expensive to make through innovation at the component level (such as sensor technology), at the systems level (through effective integration of multiple components, architecture and software) and by making use of additive manufacturing processes (such as 3D printing).
It’s important here to appreciate the close relationship between device design and device manufacture when it comes to component selection for functionality and cost of parts during production. Without delving too deep into design for manufacture (DFM) – we’ll save that for another blog! – costs associated with production are closely linked to device design, including what components are going to be assembled into the finished product.
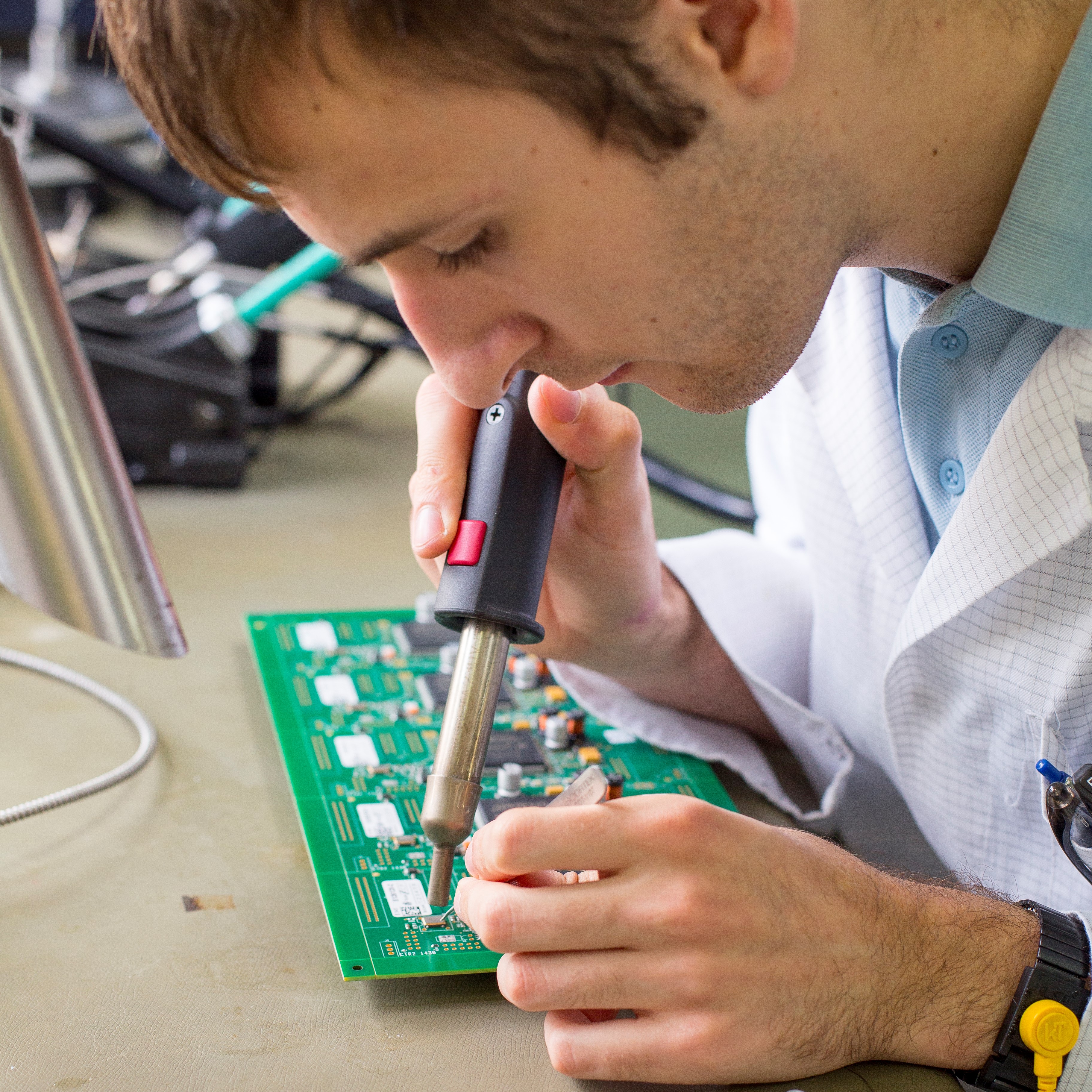
(Credit: Thomas Jull)
An example of device cost savings at the component level is highlighted in an article on chip technology by Peter Peumans. He explains that Apple’s A9 chip has more than three billion transistors but only costs $22 – incorporating such powerful but low cost components into products that can be used to optically detect illness from a patient sample (say cancerous cells in the blood) would help to keep the part cost low during manufacture.
In a similar vein, the selection of manufacturing techniques and materials for a device have an effect on its end price. Through the use of 3D printing, we are seeing class III medical devices such as implants costing just a few hundred dollars to make instead of thousands via conventional methods. Not only is this shift from one manufacturing technique to another an interesting development to observe in the industry, but seeing the production of such products in a hospital environment instead of the ‘factory’ is changing the definition of who the manufacturer is; which may also lead to further cost savings down the road too.
A final word
There is no doubt that medical devices can help reduce the cost of healthcare treatment. In some fields, and for certain medical conditions, this claim is backed with evidence of successful products that have done just that. However, in other cases we’ve seen that cost of developing and manufacturing devices is much higher than the original treatment, and thus more unaffordable to the patient.
But what I think we’ve got to remember is that it’s relatively early days in terms of some of this tech – it has potential. I’m confident that the rising cost of healthcare will continue to fuel a wave of innovation in the medical device arena, where the diagnosis and treatment of disease along with health awareness should constantly be evaluated. The boundary of what defines the medical device industry shall become more open as it works with other fields to provide us with the healthcare system of the future.
So, going back to my original question ‘Can medical devices help reduce the cost of healthcare? My answer is yes. I’m optimistic about the ability of our medical innovators to bring in solutions that will make healthcare more affordable for families in the U.S. – and importantly, beyond cost and bottom line, I believe these innovations will improve patient’s quality of life too.
References
Diagnostic and Intervention Cardiology (2016) ‘New Study Demonstrates Cost-Effectiveness of Watchman Device’, available from: http://www.dicardiology.com/content/new-study-demonstrates-cost-effectiveness-watchman-device [18 Oct 2016]
Lewandrowski E. L., Lewandrowski K (2013) ‘Implementing point-of-care testing to improve outcomes’, Journal of Hospital Administration, 2013, Vol. 2, No. 2, [online], available from: http://www.sciedu.ca/journal/index.php/jha/article/viewFile/1553/1325 [14 Oct 2016]