Telehealth, the use of TV and computer monitors to deliver healthcare remotely, is proving to be a valuable addition to many practices. Recently, a commentary on the role of telehealth in disaster response, by Brendan Carr, MD, Associate Dean of Healthcare Delivery Innovation at Jefferson (Philadelphia University +Thomas Jefferson University), and Nicole Lurie, MD, Massachusetts General Hospital, was published in The Journal of the American Medical Association Internal Medicine (JAMA Internal Medicine). The authors discuss the advantages of using telehealth during disasters and some of the barriers to widespread implementation.
Here, Dr. Carr provides a vision for what disaster relief could look like if telehealth were implemented and also discusses some of the barriers to implementation.
Q: How is telehealth used today?
While telehealth programs originally developed in rural areas, which often lack health facilities or specialists, it has grown to improve delivery of care in any medical setting, regardless of geography. Examples of telehealth now include emailing your doctor, video-chatting for follow-up visits or even urgent care, remote consultation with a specialist, and mental health screening and care. Though hands-on care cannot be replaced, telehealth provides options when a clinician cannot be physically present with a patient, or even when a visit is not required to get the right care.
The treatment of acute stroke patients is a well-known example of particularly valuable telehealth – emergency departments without stroke neurologists can arrange rapid virtual consultation in order to make decisions about clot busting drugs so that optimal treatment can be delivered as quickly as possible. Similar remote access to specialists has improved outcomes for patients in intensive care units, has been used to improve care of Zika patients in Puerto Rico, and provided mental health care to patients suffering from the water crisis in Flint, Michigan. The Department of Veterans Affairs (VA) and the Department of Defense (DOD) have substantial telehealth portfolios and have both announced expansions to their current telehealth systems that will take place this year.
Q: How can telehealth improve disaster response?
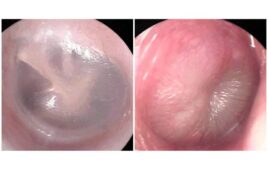
During and after a disaster, local hospitals and clinics can become overwhelmed with a massive influx of patients. In these situations, telehealth can aid clinicians on the ground to facilitate more rapid evaluation, diagnosis, and communication with patients. With remote access to subspecialists, clinicians have ready access to information that will help them stabilize, triage, and effectively treat patients with highly acute conditions. Using their own personal devices (smartphone or computer), patients in need of less intensive and immediate care can directly access providers without traveling to an already crowded hospital. Easy access to care is especially important for averting long-term mental health issues, which are rarely addressed during disaster response. Telehealth can also aid in near real time provider-to-provider education of post-disaster medical problems, such as skin conditions and infectious disease. All of these efforts can save lives and improve health outcomes for patients and the community. Apart from direct benefits to patients and clinicians, telehealth can significantly lower disaster response costs because remote clinicians do not need to be transported, fed, or housed.
Q: What are the barriers to using telehealth during a disaster?
The biggest barriers to using telehealth during a disaster are administrative and reimbursement issues. While access to electricity and internet or cell service is a barrier to telehealth in many settings, during a disaster, specialized equipment with satellite connection and batteries can be used effectively to keep on-site clinicians connected to telehealth resources. (Though limited access to electricity and internet is a barrier to patient-initiated telehealth.) Administrative barriers such as patient confidentiality, data security, licensing of telehealth providers, and reimbursement from insurance companies and disaster funds cannot be addressed with technology alone and require a coordinated effort across key stakeholders. Ideally, information about disaster-related healthcare visits could be transmitted to the patient’s regular healthcare team after the crisis in a smooth and secure manner.
Q: How can communities prepare for using telehealth in a disaster situation?
Few disaster response mechanisms work when if they are implemented for the first time during the crisis. It’s important for communities to assess their local services that may be overwhelmed during a disaster and determine exactly how telehealth could aid those services. Bolstering or expanding technology resources with an eye to using telehealth will put valuable tools in place, but communities can also identify existing technology that can be used or repurposed for telehealth during a disaster. Most importantly, communities must work with health insurers, NGOs, and federal disaster relief agencies to figure out how telehealth services will be used during a disaster.