In any healthcare facility, Infection prevention is a critical task that requires diligence. Establishing clear protocols is important, but the effort can’t stop there. There also needs to be a smart plan around developing and maintaining staff compliance. Luckily, there are a multitude of tools available to keep everyone on track.
To learn more, Surgical Products interviewed Sara Owens, clinical programs manager at PDI.
Healthcare facilities are often forced into reactive modes when it comes to incidents like lapses in infection prevention protocols. What steps can they take on the front end to avoid such situations?
One way to ensure that infection prevention protocols are being followed is through frequent auditing. Audits can be performed on many clinical tasks to help identify non-compliance before an incident occurs. It’s important that the information gathered in an audit be shared with the clinician as soon as possible so a plan can be developed to re-educate.
Some audits can be tedious and require extra resources. However, they are incredibly beneficial when attempting to identify potential risks. Some of the most important audits include hand hygiene compliance, surface disinfection protocols, and Operating Room Time Outs.
What are some of the practical considerations that must be taken when introducing and implementing infection prevention and compliance education programs?
One of the biggest things to take into consideration when introducing and implementing education programs is the amount of resources and time needed. As everyone knows, clinicians are being pulled in every direction and finding time for additional learning can be challenging. This means having a flexible structure and schedule for requirements is very important, in addition to measuring the outcomes of the program – using baseline questions like, did the education improve practice? Or, was it well received by staff?
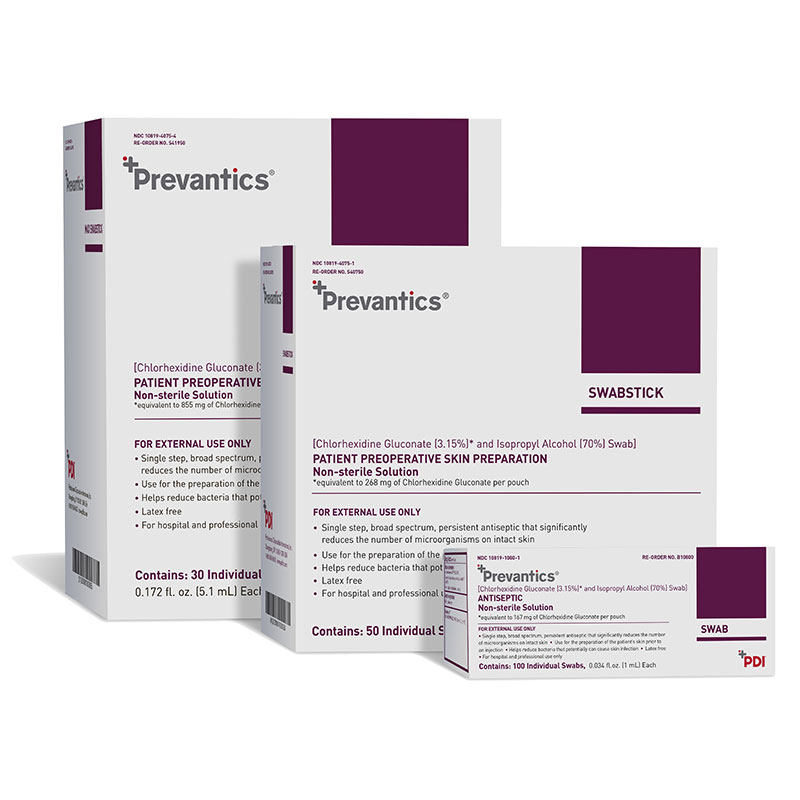
PDI’s Prevantics line includes applicators that are premoistened and ready-to-use.
What tools can facilities use to make sure certain protocols are being followed consistently?
There are several LEAN tools that can be used to help ensure compliance. Gemba rounds is one way to actually go to the place where the work is being done, to visualize and discuss the practice. An Abnormality Tracker can be used to identify any trends in non-compliance and help determine the root cause. Furthermore, Standardized Work is a great way for clinicians to follow protocols consistently. This is typically a step-by-step guide that can be easily referenced and followed by all clinicians, every time.
What approach should be used to bring staff onboard with a new plan?
Staff will always have a certain amount of resistance to change. Helping them understand the “why” is a critical element for getting them to buy in. Also, it’s essential to remind them that auditing is not trying to catch them doing something wrong, but rather a necessary step in keeping patients, and themselves, healthy and safe.
Anything else you’d like to add?
Transparency of audit results and findings, plus not forgetting to celebrate when things are being done well, is incredibly important for continuous improvement.




