Earlier this year, Surgical Endoscopy published a study showing chronic gastroesophageal reflux disease (GERD) can be effectively treated over the long-term with the Transoral Incisionless Fundoplication (TIF) procedure. Now dubbed TIF 2.0, the minimally invasive procedure employs the EsophyX device from EndoGastric Solutions.
To get more information on TIF 2.0 and the recent research, Surgical Products interviewed Karim Trad, MD, the principal investigator on the new study.
In your view, what’s the most important takeaway from the new study?
The most important takeaway of the clinical data resulting from the study is that it demonstrates the ability of the Transoral Incisionless Fundoplication (TIF) 2.0 procedure to provide sustained control of chronic gastroesophageal reflux disease (GERD) symptoms for up to three-years post-procedure.
At the three-year post-procedure mark, 83 percent of patients experienced elimination of regurgitation and atypical GERD symptoms, and 70 percent of patients had completely discontinued proton-pump inhibitor (PPI) use, confirming the TIF 2.0 procedure is a durable alternative to PPI therapy and more invasive anti-reflux surgery operations. This data further supports the growing body of clinical evidence for the TIF 2.0 procedure as an effective treatment option to improve outcomes in patients suffering from GERD.
What’s unique about the TIF 2.0 procedure?
The TIF 2.0 procedure uses a unique approach to treat the underlying cause of GERD. The EsophyX device used endoscopically for the procedure rebuilds the antireflux valve and restores the body’s natural protection against acid reflux. Using this innovative method, physicians can perform a partial fundoplication through a transoral approach, delivering effective results without the side effects typically associated with more invasive anti-reflux surgery operations. Most patients who undergo the procedure experience less discomfort, faster recovery, and fewer adverse events, allowing them to get back to life sooner, free of the distraction and discomfort of GERD.
Additionally, a high-quality clinical research program aimed at furthering understanding of GERD and improving patient outcomes supports the procedure. Over 70 peer-reviewed papers report consistent outcomes across a range of measurements including symptoms, quality of life scores, cessation of PPI therapy, and improvements in pH measurements in over 1100 unique patients.
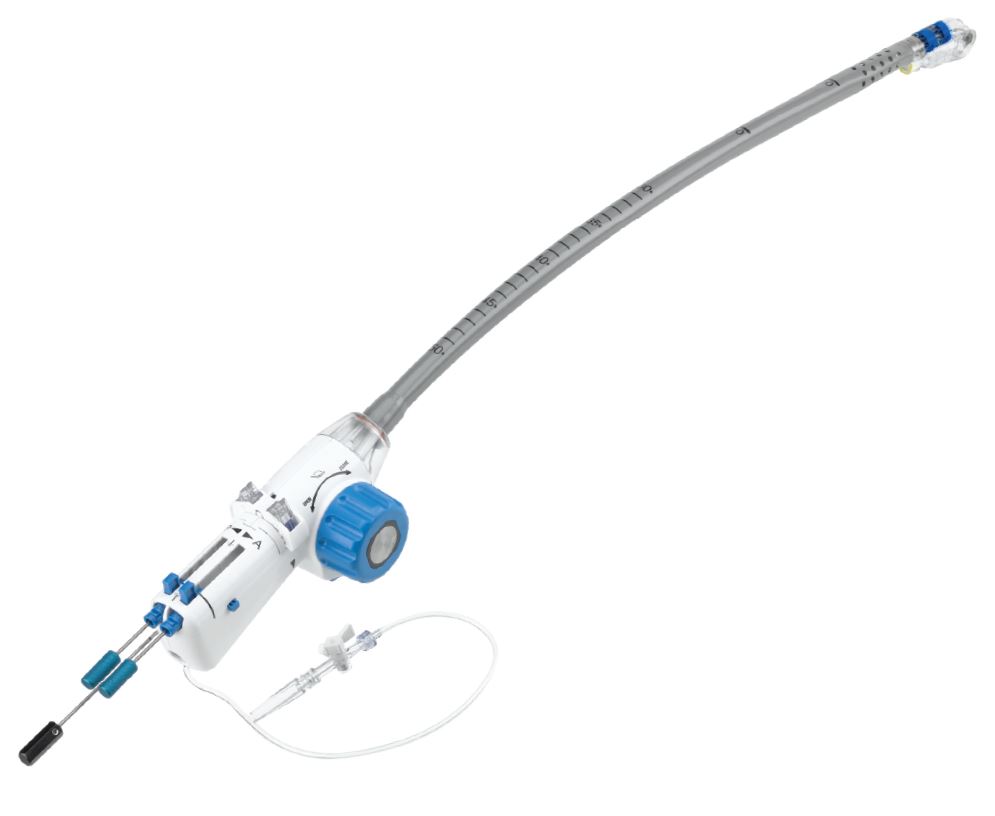
The EsophyX2 device enables the creation of a 2-3 cm, 270° esophogastric fundoplication by using proprietary tissue manipulating elements and 12 or more full-thickness polypropylene fasteners. The device is used in conjunction with a flexible video endoscope, which provides visualization throughout the TIF® procedure. (Image credit: EndoGastric Solutions)
For surgeons who want to explore TIF 2.0 as a treatment option, what should they know about transitioning to that approach?
The TIF 2.0 procedure is a unique solution for patients suffering from chronic GERD that corrects the underlying cause of the condition, an anatomic defect at the gastroesophageal valve (GEV). The procedure differs from traditional fundoplication procedures because it is performed through the patient’s mouth, rather than through laparoscopy or open abdominal incisions. The TIF 2.0 procedure is best suited for patients with a small hiatal hernia, less than or equal to 2 cm and for patients with a BMI of 35 or less. The TIF 2.0 procedure has been performed on more than 18,000 patients worldwide. Clinical data continues to demonstrate minimal postoperative side effects such as dysphagia, gas bloat, and flatulence.
Is there anything else you expect to glean from the data you’ve collected or any further research you’re hoping to do around the procedure? In other words, where do you go from here?
The investigators are collecting even longer-term follow-up data from the TEMPO study to add to the existing clinical evidence. Additionally, I participate in the U.S. TIF registry, which is also collecting long-term follow-up data. The American Gastroenterological Association is enrolling and treating patients in a unique registry that will compare the TIF 2.0 procedure to traditional Nissen fundoplication. Patient access to the TIF 2.0 procedure will become widespread as public and private payers review their coverage policies in light of this and other studies.




