Now that 3-D printing has made it easier to generate custom-made prosthetics, bioengineers are looking ahead at manufacturing actual cellular material. Such technology could be the basis for personalized biomedical devices; tissue-engineered skin, cartilage, and bone; or even working bladders. In a Trends in Biotechnology special issue on biofabrication, publishing August 17, researchers review and consider the progress made in 3-D bioprinting and what might be possible in the decades, or years, ahead.
1. Made-to-Order Organs-on-a-Chip
“Organs-on-a-chip,” 3-D microengineered systems that mimic the structure and function of human tissue, are a strong contender in the race to deliver inexpensive and efficient personalized medicine. Lung, gut, and pancreatic tissue have already been grown from human stem cells on the chips, which allow researchers to study physiological differences in these cells between patients as well as screen for drugs. Manufacturing challenges exist to quickly expand the use of the technology, but 3-D printing could reduce the labor and costs necessary to build, seed, and meet the demand for chips.
2. Skin Manufacturing
Printed skin made from cells set down on a collagen gel showed the presence of intercellular connections and biologically normal cell markers 10 days after cultivation. In another study, researchers have been able to grow blood vessels in this sheet of cells. Skin bioprinting is closer to reality than one would think, but researchers are only at the beginning of considering the designs necessary to help patients, especially those with burns or chronic wounds.
3. Facial Reconstruction
While bone, cartilage, skin, muscle, blood vessels, and nerves have all been printed in the laboratory, constructing more complex designs that can be implanted in patients is still in development. Craniofascial reconstruction, which would benefit people with cancer or who have experienced facial injuries, seems to be an obvious candidate to pursue because of the amount of work already done on these cell types. In the short term, 3-D printed scaffolds could be used to improve spot defects in the jaw or other areas of the face.
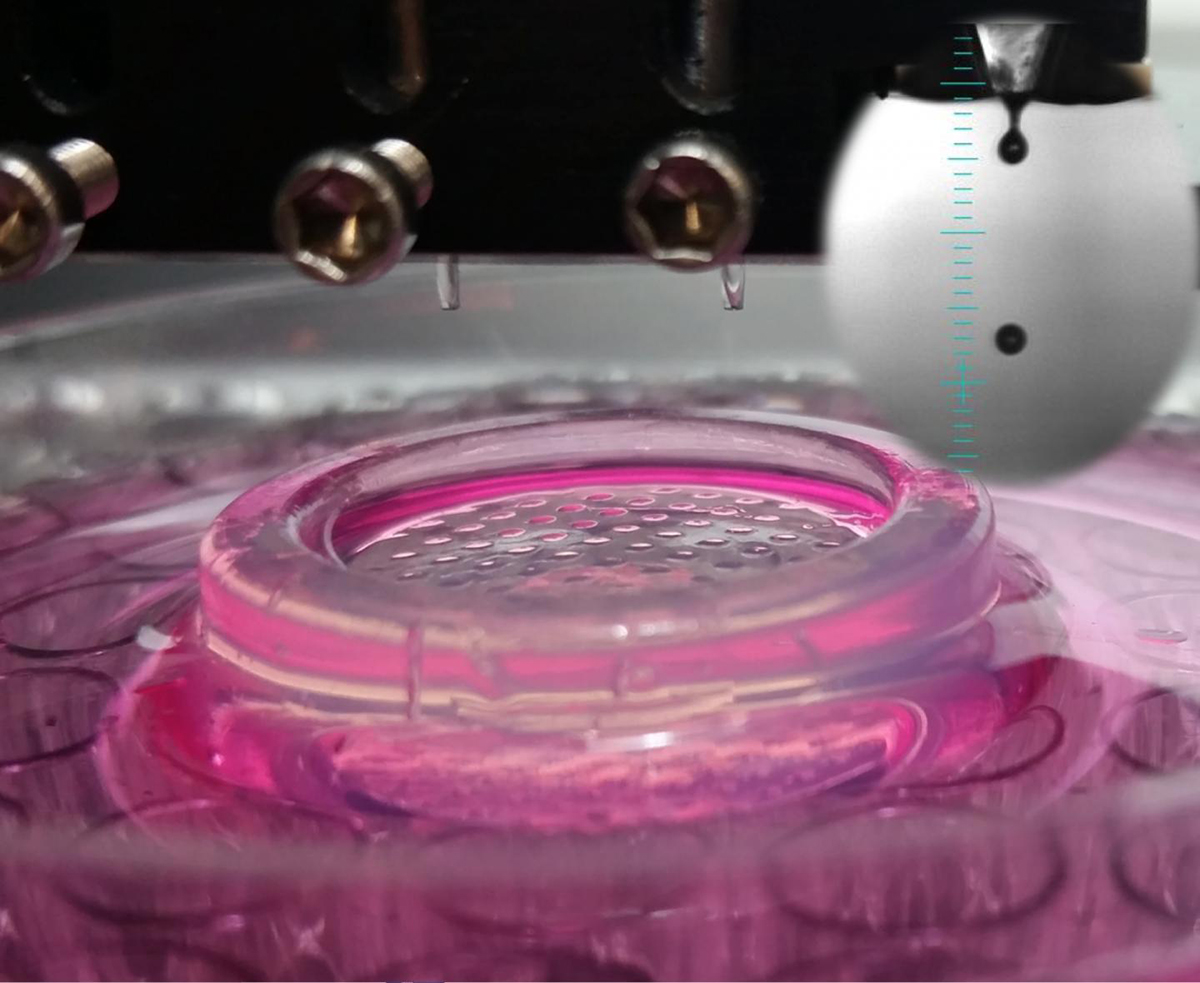
This photograph shows high throughput bioprinting of cells into microwells. (Credit: Ozbolat Lab at Penn State)
4. Multi-Organ Drug Screens
3-D bioprinting is demonstrating that precise models can improve the way we evaluate new drugs, such as by generating “organoids” made up of multiple cell types, as well as a tumor model with engineered blood vessels. While such approaches could make it possible to quickly monitor drug interactions in real time in multiple organs, much more iteration (e.g., adding blood vessels, connecting organ models) will be needed to realize this vision.
5. Plug-in Blood Vessels
Efforts to create 3-D blood vessel networks within bioengineered tissues–which would be necessary to ensure tissue survival after implantation and an accurate replication of human anatomy–have focused on stacking 2-D layers of cells or bioprinting 3-D networks, which allows for high levels of spatial control. One challenge is to create tissues with blood vessel networks that could directly connect to a patient’s arteries or veins.


