Immune system cells linked to allergies also turn out to direct healing of mouse muscle wounds when paired with biologic “scaffolding” to support them, researchers from Johns Hopkins and the Kennedy Krieger Institute report. The finding, described in the April 15 issue of Science, adds to evidence that the immune system is key not just to fighting infectious and other diseases but also to kick-starting healing after an injury. They also indicate that so-called biomaterial scaffolds can more effectively spur healing if designed to “partner” with immune cells, the researchers say.
“In previous research, we’ve seen different immune system responses to the same biomaterial implanted in different tissues or environments, and that got us interested in how biomaterials might stimulate the immune system to promote regeneration,” says Jennifer Elisseeff, Ph.D., professor of ophthalmology and biomedical engineering at the Johns Hopkins University School of Medicine. “We still have a lot to learn, but this study is a step toward designing materials to elicit a beneficial immune response.”
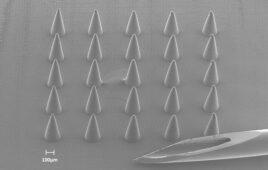
Elisseeff’s research group designs biodegradable scaffolds, made of materials such as collagen, that have shown promise in promoting regrowth of damaged tissue, in part by giving the body’s own stem cells a place to anchor and begin their work. But in the past few years, she says, other research groups have found evidence that such scaffolds could also spark healing activity from immune cells.
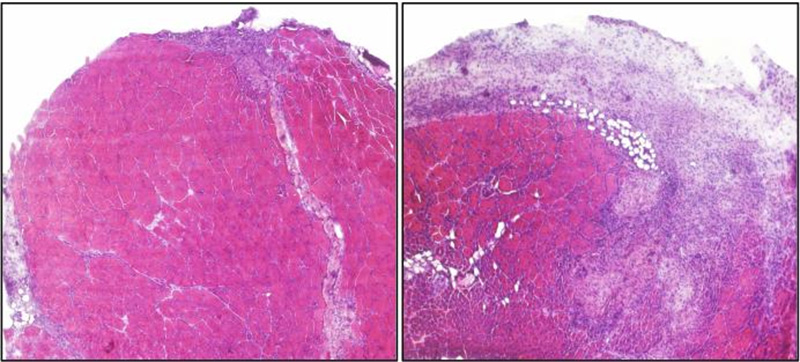
This is a cross-section of injured mouse muscle tissue, with healthy tissue in pink and scar tissue shown in purple. Both mice genetically lack T cells; the mouse on the left was injected with T cells that became type 2 helper T cells and aided healing. Photo: Kenneth Estrellas/Johns Hopkins Medicine
To learn more about the immune cells involved and their response, then-graduate student Kaitlyn Sadtler, Ph.D., worked with other researchers in Elisseeff’s lab and specialists in cancer immunology. They surgically removed part of the thigh muscles of mice and implanted scaffolds known to promote healing in animals. After a week, wound sites with scaffolds had more white blood cells than did wounds without scaffolds, and many of those cells were churning out a chemical signal, interleukin-4, that is frequently produced by so-called type 2 helper T cells.
To see what the role of those cells might be, the team did the same procedure on mice genetically modified to lack T cells and found that their wounds didn’t ramp up interleukin production or heal as well as those of the normal mice. Further investigation revealed that one role of the type 2 helper T cells was to activate and train another type of immune cell, called macrophages, at the wound site. “The T cells tell the macrophages how to behave, making them pro-regenerative macrophages,” says Sadtler.
Previous studies suggest several key healing roles for the macrophages: cleaning up dead or damaged cells and other debris, recruiting and supporting adult stem cells that regrow tissue, and sparking the construction of new blood vessels to fuel new tissue in the area. But the pivotal role of type 2 helper T cells in scaffolds comes as a surprise, Elisseeff says: Those cells help fend off intestinal worms, but in the developed world, they’re most often associated with triggering “bad” immune responses, such as allergies. “It’s interesting to see something useful coming out of this pathway,” she says.
Elisseeff notes that there is still much to learn about how immune cells respond to various kinds of biomaterials that might be used as scaffolds — an area her team continues to investigate.
“This study, in demonstrating for the first time the central role of T cells in mediating the tissue regenerative process, is truly groundbreaking,” says Drew Pardoll, M.D., Ph.D., the Martin D. Abeloff Professor of Oncology in the Johns Hopkins’ Kimmel Cancer Center and director of the Bloomberg~Kimmel Institute for Cancer Immunotherapy, who collaborated with Elisseeff on the study. “I predict it will be viewed as an inflection point, where regenerative immunology goes from an idea into a field of serious study. And it opens the door for totally novel strategies to significantly enhance tissue regeneration.”