One of the top priorities for today’s perioperative staff is maintaining normothermia throughout the patient’s surgical experience. It is well known that inadvertent perioperative hypothermia continues to be a significant challenge for patients undergoing surgical procedures, in spite of the efforts of the Surgical Care Improvement Project (SCIP).
According to a recent article in the Association of periOperative Registered Nurses (AORN) Journal, up to 70 percent of surgical patients experience inadvertent hypothermia. Potential complications resulting from perioperative hypothermia are well documented and can be life threatening, increase the cost of care and dramatically impact patient satisfaction.
The Surgical Care Improvement Project (SCIP), a national quality improvement initiative, was created in 2009 through a partnership with the Joint Commission, the Center for Medicare and Medicaid Services (CMS), and several other healthcare organizations. The overall goal of SCIP was to improve surgical care by significantly reducing surgical complications.
SCIP-Inf-10 was specific to preventing inadvertent hypothermia in the perioperative area. However, Joint Commission retired the SCIP-Inf-10 measure set effective January 1, 2014, and CMS removed the measure from the Hospital Inpatient Quality Reporting (IQR) Program beginning January 1, 2014, as well. Measures are removed because the performance is determined to be “topped out” with no meaningful difference in performance between providers and little opportunity for further improvement.
Intraoperative hypothermia is estimated to occur 50 percent to 90 percent of the time, with 70 percent of these patients arriving in the PACU hypothermic. AORN’s Guideline for Prevention of Unplanned Patient Hypothermia states that “Core body temperature is normally tightly regulated by the body, but this regulatory mechanism is altered by general, epidural, and other regional anesthetic agents and by environmental factors during the perioperative experience that can result in unintended hypothermia.”
According to AORN, hypothermia is defined as a temperature lower than 35˚ C or 36˚ C (95˚ F or 96.8˚ F). There is not a definitive value for hypothermia because research findings vary. Each perioperative area should have a policy that states their definition of hypothermia and specific criteria that activate hypothermia protocols.
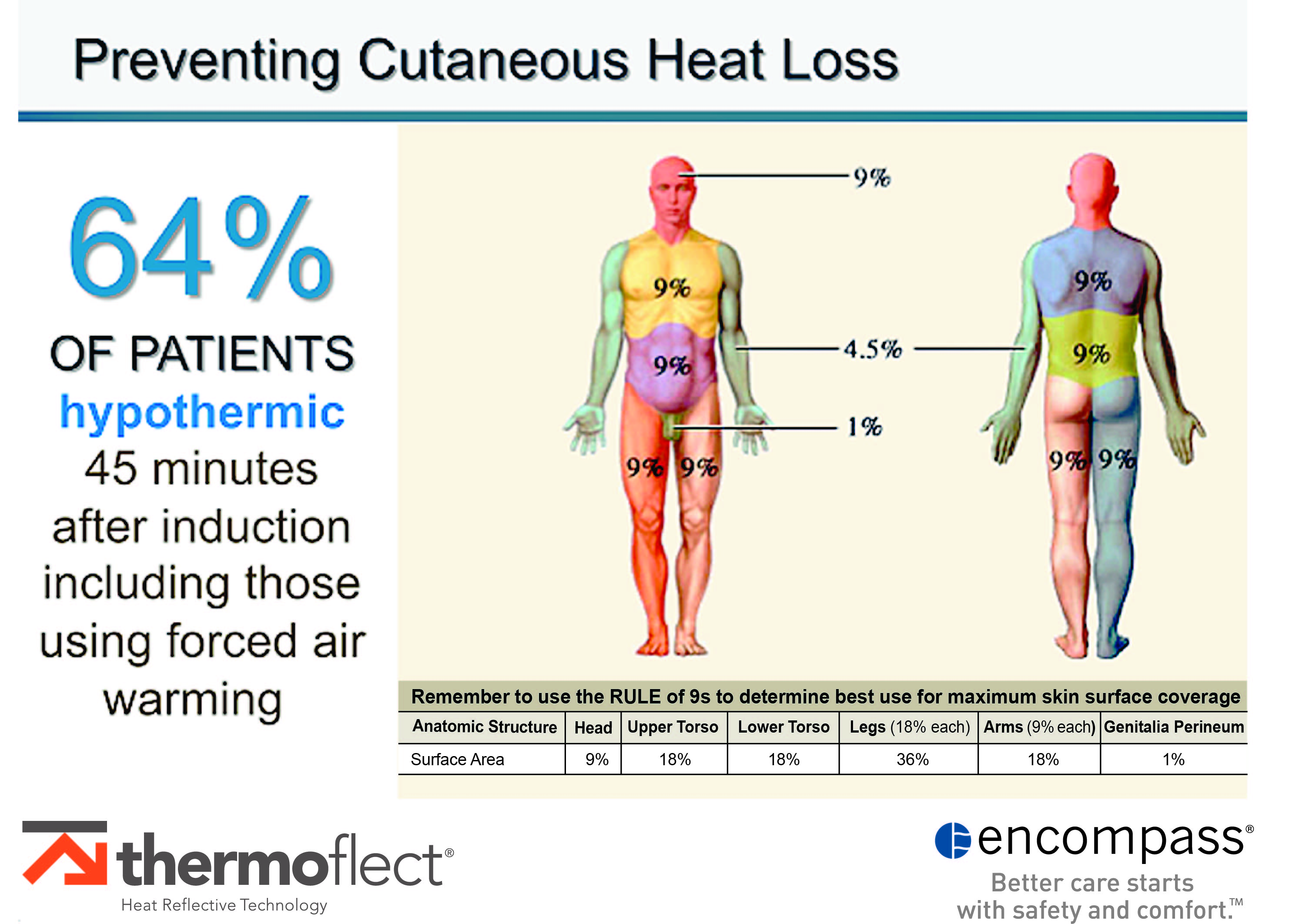
The greatest proportion of temperature decrease is attributed to the core-to-peripheral redistribution of body heat which primarily occurs during the first hour of general anesthesia and is difficult to treat intraoperatively. In a 2015 study conducted by the Cleveland Clinic which included more than 58,000 patients, it was determined that despite the use of forced air warming intraoperatively, 64 percent of the patients were hypothermic 45 minutes after induction.
A significant environmental factor involves exposure to cold room temperatures throughout the perioperative suite, which contributes to cutaneous heat loss. Administration of room temperature IV fluids also plays a significant role in cooling the patients preoperatively.
Cutaneous heat loss can occur in a multitude of ways. If the room temperatures within the perioperative area are cold, cutaneous heat loss can begin in the waiting area before the patient enters the preoperative department. Once in the preoperative department, removal of clothing and administration of cool, room temperature IV fluids are contributors to the gradual cooling of the core temperature.
When patients are transported to the operating room in this scenario, the reduction in core temperature has already begun. AORN suggests that the OR temperature be maintained at 20˚C (68˚F) or above. However, it is not uncommon for the OR to be below this temperature, especially for orthopedic rooms.
Upon arrival to the OR, cold room temperatures, anesthesia induction, patient positioning, and skin preps are all contributors to a continued path to hypothermia.
According to Roth, without prewarming, “there may not be enough time for intraoperative active warming to be fully effective.”
Once this downward path has begun, it is difficult to reverse intraoperatively, even with forced air warming. For this reason, prewarming is imperative to prevent patients from cooling before anesthesia is delivered.
Roth goes on to say that “it is difficult to demonstrate an increase in core temperature from our active warming techniques (e.g., forced air warming) until at least 30 minutes have elapsed.”
Rule of Nines
The rule of nines is a method which assigns a relative value to various areas of the body surface. Although this method was designed to determine the percentage of body surface injured for burn patients, the values can reflect body surface related to heat loss in perioperative patients.
For example, exposure of an entire leg accounts for 18 percent of the patient’s total body surface, vulnerable to cutaneous heat loss when not treated with preventive measures. In gynecologic and cystoscopic procedures requiring lithotomy position, the patient can lose up to 36 percent of their body heat in the legs alone.
Protocols should include covering as much of the skin surface as possible preoperatively, intraoperatively, and in the PACU to prevent cutaneous heat loss.

Encompass’s Thermoflect Heat Reflective Technology reflects the body’s radiant heat, forming a warm cocoon of air around the patient. (Image credit: Encompass)
The goal of every surgical procedure is to maintain the patient’s temperature within a normothermic range throughout their perioperative experience. This goal can be achieved with prewarming and taking effective steps to reduce cutaneous heat loss.
A 2012 study conducted by Horn et al. concluded that prewarming for at least 10 to 20 minutes helped reduce the rate of hypothermia. Prewarming may significantly increase peripheral tissue temperature, minimize core-to-peripheral temperature gradient, and keep core temperature within normal limits.
The findings of more recent studies indicate that 30-60 minutes of preoperative skin-surface warming significantly raises both core and mean skin temperature, prevents heat redistribution, and, when appropriately combined with intraoperative warming, provides increased opportunity to avoid the risk of hypothermia and associated complications. The prewarming process should be initiated in the preoperative area.
In late 2010, The American Society of PeriAnesthesia Nurses (ASPAN) published their clinical guidelines entitled “Clinical Practice Guidelines for the Promotion of Perioperative Normothermia: Second Edition.” Interventions identified by ASPAN to address maintaining normothermia include:
- All patients receive limited skin exposure to lower ambient environmental temperatures. Room temperatures should be maintained, according to AORN and architectural standards (20˚ to 25˚ C).
- Preoperative warming is recommended for a minimum of 30 minutes which may reduce the risk of subsequent hypothermia.
- Passive warming interventions are recommended perioperatively (preop, intraop, and PACU) as a standard part of the perioperative warming protocol.
The updated AORN Guideline for Prevention of Unplanned Patient Hypothermia identifies considerations for selecting a warming method which includes: planned procedure, patient positioning, and warming equipment constraints that could limit access to the surgical site.
Furthermore, the guideline notes “the for patient warming may be the most effective approach.”
In a 2015 research project at the University of Tennessee Medical Center, Edie Patterson and Robert Heidel led a study that compared active and reflective warming methods. They found that “Each intervention used to maintain normothermia was proven to be equally effective in preventing hypothermia.”
Prevention of intraoperative hypothermia can be minimized by pre-warming the patients and by reducing their exposure to cold room temperatures that are prevalent in the perioperative space.
Encompass’s Thermoflect Heat Reflective Technology reflects the body’s radiant heat, forming a warm cocoon of air around the patient and preventing convective heat loss to the environment. Thermoflect has a four-layer construction designed to promote normothermia and help prevent hypothermia using endogenous body heat. It preserves the body’s core and peripheral temperatures.
Thermoflect products are ultra-lightweight and specifically designed to cover and conform to all body surfaces. The composite material has a soft cloth-like inner lining designed to be comfortable on the patient’s skin.
Thermoflect products are used in most patient care settings. In the perioperative area, patient gowns, blankets, caps, leggings, and staff jackets are used in patient warming protocols and provide warmth to the staff members in the traditionally cold perioperative environment. Blankets and gowns are used in patient care units to warm patients and reduce utilization of warm bath blankets and associated costs.
There is strong evidence that inadvertent perioperative hypothermia continues to occur in the perioperative setting. Minimizing cutaneous heat loss and the use of passive warming methods, such as Thermoflect Heat Reflective Technology, have been demonstrated to be an effective method for maintaining normothermia in patients throughout their perioperative experience.
Angie O’Connor, RN, BS, CLLM, is the director of clinical resources at Encompass. She began her clinical career in the perioperative arena, specializing in orthopedic and cardiothoracic surgery, and has worked as a strategic account executive for AORN.




