Management of chronic pain is one of medicine’s most intractable challenges affecting billions of individuals in the U.S. With no objective or quantifiable metric for evaluating pain, healthcare providers are forced to rely on patients’ self-reported pain levels. Too many factors in this guessing game contribute to poor – sometimes catastrophic – outcomes.
A recent market research report indicates that more than 1.5 billion people worldwide suffer from chronic pain and that approximately 3- 4.5% of the global population suffers from neuropathic pain.
The bottom line is this: pain affects more Americans than diabetes, heart disease and cancer combined. And new solutions are needed to remedy this vexing problem. Without a dependable method for pain assessment, doctors are often thwarted when it comes to patient care. Usually patients are asked to rate their pain on a scale of 1-10 (Brief Pain Inventory, BPI) or using pictorial references (Wong-Baker Faces Pain Scale). Not only are these scales useless with nonverbal patients, self-reported pain levels are fallible; personality and tolerance, cultural and gender differences, emotional resiliency, personal perception, relative experience, and addictive tendencies all affect the way individuals perceive and report their pain.
The Cost of Guesswork
The results are not pretty. Some patients – especially children, elderly and non-verbal people – suffer needlessly when their pain is underestimated and under-treated. Analgesics that provide relief for one patient may not help another. There are different types of pain in addition to the range of severity that can be experienced. Patients can build up tolerance that diminishes painkillers’ effectiveness; or they may experience intolerable side effects – with or without pain relief. When one drug doesn’t work for a specific individual, switching to a different medication can restore functionality. Making these judgment calls is difficult when the degree of suffering can’t be reliably tracked or measured.
The acute pain associated with injury or surgery sometimes progresses to become chronic, maladaptive pain (persistently experienced for longer than three months), which is exceedingly difficult to assess and treat. A waterfall of disastrous consequences often follows: many patients can’t get the relief they need and their quality of life deteriorates. Others are treated with medications that work for a while but become less effective over time. Long-term opiate use for pain management can create addiction in predisposed patients – all because doctors are not able to objectively evaluate their patients’ pain levels or the effectiveness of the medications they prescribe.
The prevalence of suffering is as staggering as the negative consequences of medicine’s attempts to alleviate pain. Over 100 million people in the U.S. – a third of the population – are reported to suffer from chronic pain1. An estimated 40%-70% of them are not receiving adequate relief from medical treatment, for a variety of reasons2. Opiate prescriptions escalated so dramatically in the U.S. (peaking at 259 million in 2012), with a parallel increase in their illicit use, that regulators began working to impose limits. Fearing legal and public health repercussions, many physicians find it safer to under-prescribe than to over-prescribe opiate painkillers, which adds to the suffering of those who need them.
Epidemic Opiate Addiction and Overdoses
Under-treating pain is inhumane. Over-prescribing painkillers – particularly opiates – can be fatal.
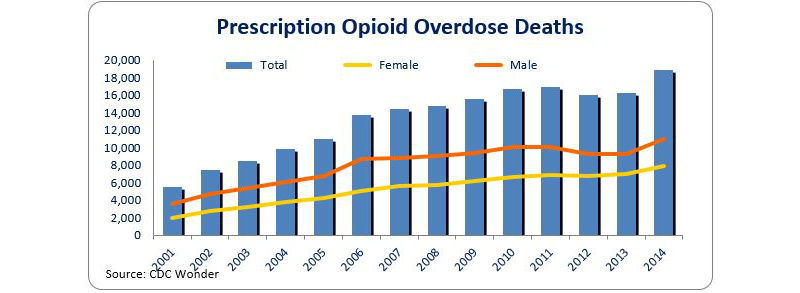
In 2014, almost 19,000 Americans died from prescription opioid overdoses.3 According to a study by the National Institutes of Health (NIH), data shows that 1.9 million Americans live with prescription opioid abuse or dependence.
Evidence shows a decrease in opioid prescriptions is leading to a new crisis as people who can’t get their opiates legally are turning to heroin, which is cheaper and in some communities, more easily obtained.4 In addition to those who died from prescription opiate overdoses, nearly 11,000 Americans died of heroin overdoses in 2014 – a 6-fold increase from 2001. This growing epidemic of heroin use and sadly, overdoses and deaths, is now at the top of many communities’ public safety concerns.
There Has to Be a Better Way
Research on the origins and mechanisms of pain is ongoing, including work to develop new technologies that can provide the information that doctors need. From this research comes clear evidence that while pain generally originates with injury, it is experienced in the brain. The search for solutions to address the experience of pain is intense. A number of approaches are in use, but there is no silver bullet for the challenges associated with pain management. Abuse-deterrent formulations promise the ability to use opioids in ways that resist or discourage abuse, whether through manner of ingestion or physical and chemical barriers. However, the challenge remains preventing dependency on opioids for relief5. Another treatment known as Transcutaneous Electrical Nerve Stimulation (TENS) is a therapy that uses low-voltage electrical current for pain relief. This method of treatment avoids the use of drugs for pain management, but experts have questioned its overall effectiveness in treating chronic pain6 and the long-term impact it can ultimately deliver7.
A more viable approach is to accurately measure pain before pain management solutions are even prescribed. An accurate measurement of pain will enable vast improvements in treatment and all of its repercussions. Health care providers will be empowered, with objective assessment, to prescribe appropriate pain killers where needed, to evaluate their effectiveness, and to reduce the risk of enabling active addiction.
The use of a wearable medical device to measure pain through the acquisition of direct biosignals that quantify the nervous system’s response to pain is one such alternative to traditional methods. A wearable medical device that provides an instantaneous, real time, numeric readout indicating a level of pain (or the absence of pain) and transmits pain measurements wirelessly can enable healthcare providers to track and analyze a patient’s pain level and their response to treatment. With more proactive monitoring and seamless data transmission between them, both doctor and patient can gain a clearer understanding of the appropriate means of treatment.
“Medical device companies are going in the right direction when they enable real patient benefits and in the case of pain measurement, the payoff is even greater,” said Ken Fine, president and founder of Proven Process Medical Devices. “When healthcare providers can objectively quantify their patients’ pain levels, the benefits will extend well beyond patient care. These advancements will provide a positive path forward for improving quality of life for billions of people while helping to stem the growing scourge of addiction and preventing deaths.”
A Hopeful Future
Millions of lives will be substantially improved, and many thousands saved, with the advent of accurate pain measurement. Doctors will breathe easier, patients will receive more appropriate treatment, and addictions will be prevented when it becomes possible to know for sure whether opiate medications are needed, if they are working, when other treatments should be considered, and when a prescription drug becomes a problem, instead of a solution.
Effective pain management should be a basic human right, and doctors should be willing and able to eliminate their patients’ suffering confidently in the knowledge that they’re helping, not endangering, lives. With technology that delivers the granular intelligence doctors need to build an informed response and approach to pain management, the potential exists for a paradigm shift in reducing drug dependency and enhancing patient quality of life.
References
1Institute of Medicine 2011 Report, Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research
2National Institutes of Health. Pathways to Prevention Workshop: The Role of Opioids in the Treatment of Chronic Pain. Draft Executive Summary. September 29–30, 2014.
3NIH, National Institute on Drug Abuse,, http://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates
4http://www.drugabuse.gov/publications/research-reports/relationship-between-prescription-drug-abuse-heroin-use/introduction
5http://www.nytimes.com/2015/06/07/us/painkillers-resist-abuse-but-experts-still-worry.html?_r=0
6http://www.webmd.com/back-pain/news/20091230/tens-gets-thumbs-down-as-back-pain-treatment
7http://ptjournal.apta.org/content/93/10/1397.full)