Providing advanced medical care in a patient’s home once required the help of trained professionals. No longer – new sensor technology is enabling a massive migration from hospitals to home care environments.

Outset Medical’s Tablo home hemodialysis platform features a streamlined touchscreen interface and a small size. But the real core of its effectiveness lies in its sensors. [Image courtesy of Outset Medical]
Medtech is on the move again. New technological advances are enabling systems that have, for years, been shackled to hospitals and clinics, to travel home with their users.
For decades, hemodialysis systems have been limited to use within highly-controlled and monitored healthcare environments, but new developments are helping change that paradigm.
What’s at the heart of that change? Sensors.
Improvements in sensor technology have been an “absolutely vital advance” for home hemodialysis platform developer Outset Medical, CEO Leslie Trigg told Medical Design & Outsourcing. Though the device features a streamlined touchscreen interface, a small size and other factors that may impress patients and doctors alike, the real core of its effectiveness lies in its sensors.
“The backbone of simplicity starts with sensors and software,” Trigg said.
The industry is taking note. Investments in home hemodialysis tech have been on the rise; last year, Fresenius Medical Care put in a $2 billion bid to acquire home hemodialysis developer NxStage Medical.
Over the past three years, Outset Medical brought in more than $200 million to support its Tablo platform. Advances in sensor technology have been essential in the development and success of Outset’s platform, Trigg told us.
“The Tablo is sensor-rich in its construction, in its design. We’ve been able to effectively use sensors to automate not only the treatment management, but the maintenance of the machine, and make the whole experience from beginning to end less labor-intensive for the patient. And when something is less labor-intensive, the cognitive burden is lower, and then when the cognitive burden is lower, you expand the number of people who can capably manage their own [treatments] using the technology,” she explained.
Advances in sensor technology are driving more change than just in hemodialysis care, according to TE Connectivity’s Pete Smith. They’re also changing how medtech developers think about care across the spectrum, said Smith, senior manager for sensor product knowledge & training.
“I’ve been in the sensor industry for 47 years, so I’m kind of the old man of the place,” Smith, a 32-year TE Connectivity veteran, said. “For a few years now, the medical industry has been trying to move patient care out of hospitals and into the home for a number of reasons – things like the fact that people are more comfortable in the home, they’re surrounded by people they know and they get as good care as they would in the hospital.”
As patient care moves toward the home, so too must the machines necessary to their care and survival. This includes simple devices, such as diagnostics and monitors, and more advanced machines such as hemodialysis systems.
“Because it’s more convenient for the patient, it’s easier to do. They can schedule around their availabilities,” Smith told MDO. “Better scheduling means an increase in compliance, which can be critical to the well-being of patients undergoing hemodialysis.”
And self-managing care comes with other advantages, Outset CEO Trigg said.
“We’ve seen this in other fields – diabetes is one that comes to mind immediately. It’s a case where putting the patient in charge of their own care has absolutely lowered the event rate, lowered hospitalization rates, lowered ER visits. And I think a similar movement is likely to hit dialysis, finally,” she said. “We know that the more you miss dialysis, the higher your risk for hospitalization and ER visits. So simple things like that – the patient missing fewer visits, and being less likely to be in the hospital.”
But it’s not as simple as sending patients home with a new appliance.
“There are things that you have to worry about when you take one of these medical machines and send it outside the hospital environment. First of all, when it’s in the hospital, it’s being operated by a professional – someone highly trained who knows how to work it, understands indications on the machine and can determine if it’s not working right,” Smith noted.
Hospital equipment isn’t generally designed with the layperson in mind, he added, and the indicators and data they display often requires medical training to interpret.
“If it’s not effective, or there’s some problem with the treatment the machine is delivering to the patient, professionals at the hospital will quickly recognize that,” Smith said.
For decades, this requirement has limited home care to those who can afford a trained attendant along with the equipment. But that’s beginning to change due to advances in sensor technology, he said.
That technology allows equipment engineers to streamline the care process and design machines that don’t require advanced medical training to be safely and effectively operated.
“To make this work, the machine has to be aware of the patient’s situation. What is the status of the patient, what are their vital signs?” Smith explained. “They collect that information regularly in the hospital, but how do they do it at home? The machines have to be designed not only to do their job, but to monitor all of the various physiological parameters that are important to a recovery procedure, the recovery process for the patient. And much of this awareness that the machine has to have is delivered from sensors.”
For applications in home hemodialysis, this includes advanced blood pressure sensors, temperature sensors and flow sensors, among others, Smith said.
At Outset Medical, a wide array of sensors were necessary to enable the system to provide home-based care.
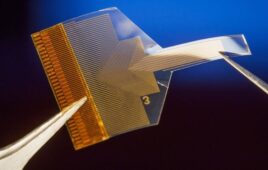
“To power Tablo’s unique functionality, conductivity, temperature, pressure and ultrasound sensors are key. For example, conductivity sensors are essential in quantifying Tablo’s real-time water purification performance, ensuring that the dialysate is mixed properly and confirming the patient has set up the concentrates correctly. Ultrasonic sensors are important for detecting fluid versus air in lines, which helps enable automated priming and prompting the machine to proceed to the next step. These sensors also provide indispensable patient safety protection,” said Outset Medical COO Martin Vazquez.
Beyond monitoring patients’ status, home equipment has an even harder job – monitoring its own status.
“There’s a second feature that these sorts of machines have to worry about, and that’s its own health. The machine needs to be aware of it, it needs to know if it’s operating properly. It needs to be able to determine, in its role as a machine to the patient, ‘Am I doing the right thing, the therapy that the doctors ordered?’” TE Connectivity’s Smith said.
This requires, essentially, an entirely different set of sensors intended to monitor the device’s safety and effectiveness. And in a world where malfunctions can mean actual life-or-death consequences, those sensors play a vital role.
“There’s a whole set of sensors inside these machines that essentially monitor only the machine operation,” Smith said.
This includes another separate set of pressure and temperature sensors, flow sensors and even simple things like balance and stability monitors, Smith said. It’s also important that machines like this can identify internal or non-obvious damage.
“You’re actually not only monitoring the health of the patient, but you’re also monitoring that the machine is accurately monitoring the health of the patient, and simple things too, like if the machine was dropped on the floor, was it dropped hard enough that it might have caused damage?” Smith said.
On top of self-monitoring, home-care devices also need to be simple, Smith added.
“The perfect machine designed to go home with a patient has two controls on it – an on button and an off button,” he said.
Patients can’t be expected to understand or manipulate various advanced controls that a professional in a hospital environment would be required to, as that introduces yet another opportunity for device failure.
“If you put advanced settings on a machine and give it to someone that’s not trained in it, there’s a fairly high likelihood that they’re going to set it wrong – that some agent out there will figure a way to do it wrong. So you want to minimize the number of patient controls,” Smith said.
This calls for, yet again, more sensors – to monitor the device’s condition and settings, and stop operation if incorrectly set. And if the machine can’t function safely, it can’t rely on the patient to notify the appropriate bodies – it has to do it itself, he added.
“Most of these machines are now, I believe, connected to the Internet. They have Bluetooth, they can hook up to your phone. And doctors give patients the home monitoring equipment so that once a day, or once every two days, or whatever interval the doctor directs, the machine will send all the data it has collected back to the doctor’s office where it can be reviewed and analyzed. And the machines can also send back a report saying, ‘Hey, something happened to me. I got dropped on the floor and this part of me isn’t working,’” Smith said. “These machines can turn themselves off, call the doctor and say, ‘I’m not working.’”
For Outset Medical, taking into account both software and sensor capabilities was necessary to produce a machine that could be safely operated by both inexperienced and experienced users, according to COO Vazquez.
“Our primary goal was to ensure that Tablo was easy and accessible for the broadest possible user base. To get there, we needed to design something that could be as easily used by a 70-year-old dialysis patient as by a professional dialysis nurse in an ICU. We also had to consider how to design for a new user versus one who is more experienced with dialysis,” he said. “To address the needs of an inexperienced user population, we employed three strategies.”
Those strategies are providing low information density on each screen, using animations to show each step of the process and requiring no memorization or mental math of the user, Vazquez said.
While those simplified features can be a boon for inexperienced users, they can often leave more advanced users and medical professionals wishing for more, he said.
“By contrast, advanced users are often looking for more information – they want to compress the workflow and can move to more advanced troubleshooting on their own. To ensure we also served this audience, we designed default settings to aid the inexperienced user, but included advanced features and displays behind the defaults,” Vazquez said. “In this way, we were able to keep the core Tablo experience simple and relatable without restricting the extra bells and whistles for those who want them.”
Sensor technology is still actively improving, Smith said. It’s getting smaller, more energy efficient and more capable at monitoring multiple spectrums and could enable even more advanced medical technology to travel home with its users.
“The future is that they’re trying to make all this medical equipment sort of ‘invisible,’ or at least unobtrusive,” Smith said.
For Outset’s Trigg, hope lies in the idea that this sensor tech, and the devices it enables, will allow more people to receive treatment. Currently, less and less areas in the U.S. can handle massive dialysis facilities, and many areas go under-served with the current infrastructure, she said.
“There are still many pockets across the United States of patients who are underserved, patients who are still driving long distances just to get their dialysis,” Trigg said. “It’s been really gratifying to have patient feedback, like wow, this is just so much easier, and it’s so much better and it’s made a dramatic impact on their life – that’s been really gratifying.”