“Sponges being left behind is the number one contributor to the number one surgical never event, which is retained surgical items,” says Jason Davies, senior brand manager with Stryker Surgical Safety.
According to research cited by Davies, surgical sponges are left inside of patients approximately 4000 times per year, which translates to 11 incidents per day. There is a 4.5 percent mortality rate when a sponge is left behind, and a permanent injury is the outcome 60.3 percent of the time.
These are the daunting numbers Stryker had in mind when they developed the SurgiCount Safety-Sponge System.
SurgiCount doesn’t take the place of the old fashioned practice of keeping a tally of sponges in the OR. The tool is meant to be supplemental, verifying a manual count.
Sponges tagged with a code are scanned into the system as part of surgical prep and then scanned out when they are removed from the surgical field during an operation. If they’re not all accounted for at the end, there’s a problem to solve before sewing up.

(Image credit: Stryker)
Preserving the bar code throughout the rigors of different procedures is especially important.
“The design of the SurgiCount sponge incorporates a hydrophobic layer on the barcode that wicks away fluids and blood, ensuring maximum readability before and after use,” says Nate Miersma, director of surgical safety at Strkyer. “We’ve seen countless real-life tests done by nurses during clinical trials where a sponge is intentionally soaked and coated with the worst types of fluid — the labels still repel the fluid very effectively and are able to be read by the SurgiCount scanners and tablets without issue.”
While SurgiCount is a tool that can be used by the entire surgical team, Stryker sees it as a particular boon for nurses in the OR.
“Right now, the nurses have a deficit of technology,” Davies observes. “They use a whiteboard and a marker on the wall inside the operating room, but they don’t have anything else, not even a second set of eyes or any other safety net. And they’re doing all these different things — multi-tasking, multiple shift changes, they have high BMI patients and emergent procedures.”
According to Davies, the abundance of challenging tasks and corresponding diverted attention make the argument in favor of adding another mechanism for tracking surgical sponges.
The tool tells the nurse in real time whether the sponge count is correct or incorrect, shifting the question at the end of the case from “Is my count correct?” to “Has my count been validated by SurgiCount?”
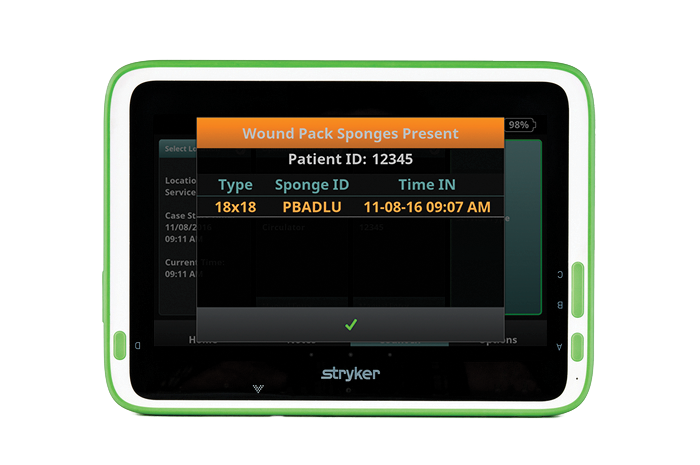
SurgiCount provides real-time tracking of sponges used in the procedure. (Image credit: Stryker)
The software previously ran on compact devices, but Stryker recently introduced a tablet version. They say it’s an upgrade that makes the platform more user friendly and intuitive.
“We wanted it to be larger — going from a 3-inch screen to a 10-inch screen — to draw in more of the surgical team into the count,” says Davies. “Everybody’s responsible for making sure the count is correct, including the scrub nurse, the circulating nurse, the surgeon.”
The tablet is designed to be attached to an IV pole, so there’s no need to find additional floorspace in a room where real estate is at a premium.
The overall intention is to make SurgiCount as easy and unobtrusive as possible, even when it comes to general utilization of the device.
“The system begins to scan and it wants to know three things: who’s the opening circulator, who’s the patient, and what sponges are going in that patient,” says Davies.
A master tag on the outside of a bundle holds the unique identities of all the sponges included in that grouping, so one pass by the scanner loads all of the individual items into the system. Once the scan takes place, the system indicates the total number of sponges, both audibly and visually.

The “Count In” screen begins the process of tracking sponges for the OR team. (Image credit: Stryker)
“When the sponges come off of the surgical field from the patient, the circulator nurse — when he or she has time — will press the ‘Count Out’ button,” Davies explains. “From there, it’s very simple. Instead of going from the field to a bucket to a sponge-counting bag, the route is: field to bucket, scan it, and then they’ll bag it.”
It further provides for an additional safeguard in the case of shift changes, items inadvertently moving between operating theaters during double-booked surgeries, and other circumstances that can introduce a potentially devastating X factor into a procedure.
Since accountability is key, all data collected from SurgiCount is immediately uploaded into the cloud.
“If you’re going to invest in the technology, you want to prove your outcomes,” says Davies. “That’s exactly what SurgiCount 360 software does. Other adjunct technologies don’t have a backend database like this.”
The collected data is a boon for healthcare administrators, providing insights on OR efficiency and a shield against malpractice litigation.
“SurgiCount 360 provides virtually unlimited customizable reports by tracking an array of metrics — including results by procedure, specific product, individual user, or facility,” says Miersma. “This allows hospitals to document results, address risk areas and replicate strengths. SurgiCount also enables administrators to identify gaps in compliance or training needs in various areas of the hospital.”
All these elements are useful, but ensuring patient safety is always the bottom line. Thus far, the system has yielded the desired results.
According to Stryker, over 540 hospitals have adopted SurgiCount. Over the course of the past six years, SurgiCount has been employed in over 11 million surgeries, tracking approximately 200 million sponges. In that vast sea of surgeries, there have been zero sponges left behind. In a statistical analysis, Stryker estimates the system has prevented approximately 1,375 retained sponges. As a result, hospitals using the system have avoided 224 permanent injuries and prevented 61 deaths.
Those numbers fuel the confidence that inspired Stryker to offer an added guarantee to SurgiCount users.
“We’ve created a program that we call the SurgiCount Promise,” says Davies. “It’s a risk-sharing and indemnification program.”
As long as the healthcare facility is using SurgiCount properly, Stryker will provide up to $5 million in product liability indemnification in the instance of a retained sponge that the system failed to protect against.
At facilities that have adopted the tool, the levels of support and protection SurgiCount provides help OR teams put the focus squarely on the patient, knowing that they’ve got an extra stopgap against a devastating mistake. They can practice medicine with a different sense of ease, accordinging to Jeffrey Pearl, MD, vice chair of the department of surgery and associate chief medical officer at UCSF Medical Center at Mount Zion.
“The Safety-Sponge System has given OR nurses at UCSF a tool they and surgeons can count on for an accurate count,” reports Pearl. “Using this system for the past two years has provided relief for the entire surgical team and eliminated this preventable and devastating event.”




