Although the figure for the growth of the transdermal drug delivery market is impressive–annual sales are expected to meet 485 million units by 2030–it’s not necessarily a surprise for those close to the industry. Transdermal drug delivery is the perfect blend of medicine and technology for a preferred alternative to conventional vaccine delivery.
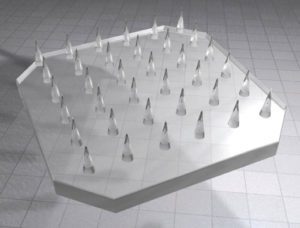
A subset of transdermal drug delivery, microneedle technology using liquid silicone rubber (LSR), provides stronger, smaller polymers that are more stable and can last longer through multiple uses. This is helping to drive the growth of the transdermal drug delivery market. We look now at manufacturing and engineering progression as part of this growth.
Microneedle solution for drug delivery
Transdermal devices can be found in multiple versions. There are patches that are placed on the skin to allow medication to be absorbed through the skin into the bloodstream. Implants are also available that create a port for medicine to be delivered. Essentially, transdermal delivery is any drug administration that involves active ingredients being delivered across the skin for systemic distribution.
Perhaps the most promising devices being introduced today use microneedles, which are divided into four types:
• Hollow. These infuse a drug through the bores with adequate flow.
• Solid. These puncture holes in the skin to increase permeability where a drug is then delivered.
• Polymer. These are made from special polymers that offer dissolving, non-dissolving, or hydrogel-forming options.
• Coated. These are coated with a drug-containing dispersion.
Transdermal devices using microneedles solve a long-standing medical problem: The skin’s anatomical peculiarities make it difficult to cross. The skin’s major barrier consists of the stratum corneum, the outermost layer. However, the layer underneath, the viable epidermis, also plays a protective role. According to research published in Pharmaceutics, only compounds that are able to get through the stratum corneum and diffuse through both layers of the epidermis have the potential to reach circulation and achieve systemic effects.
The tremendous benefits of microneedle drug delivery
One obvious benefit of transdermal microneedle delivery is that it reduces the need for hypodermic injections. Although they’re effective, hypodermic needles can cause discomfort, bruising, and even hypersensitivity at the injection site. For patients receiving an occasional vaccine, this is a minor inconvenience, but the effects are much more serious for patients requiring daily or weekly injections. A transdermal patch is virtually pain-free and can be self-administered, resulting in improved medication compliance.
In addition, improved drug delivery is often found with transdermal drug delivery, especially over an extended period. Orally administered drugs must travel through the metabolic system of the liver, which eliminates a substantial amount before widespread distribution. Lesser amounts of a drug are needed when administered through a transdermal device. In addition, a transdermal patch can deliver an even flow of the active ingredient over an extended period, ranging from 24 hours to seven days.
Many oral medicines do not absorb well in the gastrointestinal tract, resulting in low bioavailability. The bioavailability of a patch is also fairly low, but placed correctly, it can avoid first-pass metabolism and partial elimination.
Microneedle patches also permit site-specific dosing. For example, placing the patch on or near an injured appendage to reduce inflammation, rather than having the drug circulate throughout the entire body. Studies have shown that changes in the absorption and distribution of drugs administered via patches are quite different from those taken orally.
Patches also provide a new way to control a drug’s pharmacokinetics. Taking a pill once a day is relatively easy to remember, but sometimes multiple daily doses at set intervals are needed to reduce side effects or offset a metabolism issue. This is inconvenient for patients and especially difficult to manage overnight. Patches allow for exact control of both dose and time. Twice the size of a patch means twice the dosage. When you need to stop dosing, you remove the patch.
Finally, there’s evidence that transdermal microneedle methods are more effective than hypodermics for immunization. Certain cells in the epidermis and dermis (Langerhans and dermal dendritic, respectively) are part of the skin’s unique immune system. Because they’re designed to initiate immune responses to protect the body, less vaccine is needed to initiate a defense response when administered via a transdermal patch than intramuscularly.
Manufacturing and material advances
Tremendous advances have been made in recent years in the design and manufacturing of microneedles, in part due to materials technology. In particular, silicone has become an excellent option because of its haptic properties. Silicone doesn’t cause skin irritation, is biocompatible, and is compliant with medical industry regulations.
LSR technology has proven particularly suitable for transdermal drug delivery, providing small, strong polymers that are stable and long-wearing. Needle microfabrication requires parts weighed in micrograms or nanograms, and LSR allows complex, high-precision components to be produced in large volumes in these dimensions with relative ease and precise accuracy.
Ideal drug properties for transdermal delivery
Transdermal administration is not appropriate for all types of drugs. The optimal physicochemical properties of the drug and its biological properties must be considered, along with the pharmacokinetic and pharmacodynamic properties of the drug. The most important requirement is the need for controlled delivery, such as short half-life, adverse effect associated with another route, or a complex oral or IV dose regime.
The parameters for ideal candidates can be divided into physicochemical properties, biological characteristics, and polymer variables.
Physicochemical properties
• The drug should have a molecular weight less than approximately 1000 Daltons.
• The drug should have affinity for both lipophilic and hydrophilic phases. Extreme partitioning characteristics are not conducive to successful drug delivery via the skin.
• The drug should have a low melting point.
• Since the skin has a pH of 4.2 to 5.6, solutions within this pH range are used to avoid damage to the skin. However, for a number of drugs, there may also be significant transdermal absorption at pH values at which the unionized form of the drug is predominant.
Biological characteristics:
• The drug should be potent with a daily dose of the order of a few mg/day.
• The half-life of the drug should be short.
• The drug should be non-irritating and non-allergic.
• Drugs that degrade in the GI tract or are inactivated by hepatic first-pass effect are suitable candidates for transdermal delivery.
Polymer variables:
Advances in transdermal drug delivery technology have been rapid because of sophisticated polymer science that allows incorporation of polymers in transdermal systems in adequate quantity. The release rate from transdermal systems can be tailored by varying polymer composition. Selection of a polymeric membrane is important in designing a variety of membrane-permeation controlled transdermal systems:
• The polymer should be chemically nonreactive or an inert drug carrier.
• The polymer must not decompose on storage or during life span.
• Molecular weight, physical characteristic, and chemical functionality of the polymer must allow the diffusion of the drug substance at a desirable rate.
• The polymer and its decomposed product should be nontoxic. It should be biocompatible with skin.
• The polymer must be easy to manufacture and fabricate into desired products. It should allow incorporation of large amounts of active agent.
Silicone elastomer blend networks, sugar siloxanes, amphiphilic resin linear polymers, and silicone-hybrid pressure-sensitive adhesives are showing promise for potential performance advantages and improved drug delivery efficacy.
Early on, transdermal delivery systems were used mainly for delivery of small, lipophilic, low-dose drugs. More recently, delivery systems began using chemical enhancers, non-cavitational ultrasound, and iontophoresis to enhance the efficacy of transdermal patches. Today, the ability of iontophoresis to control delivery rates in real time is providing added functionality in a number of instances.
At the same time, microneedles combined with thermal ablation are progressing through clinical trials for delivery of macromolecules and vaccines, including insulin, parathyroid hormone, and influenza. With these enhancement strategies, transdermal delivery is poised to significantly impact drug delivery choices.
Both chemical enhancers and the newest physical enhancers (ultrasound, thermal ablation, and microneedles) have begun expanding transdermal delivery of macromolecules and vaccines. These scientific and technological advances enable targeted disruption of the stratum corneum while protecting deeper tissues, positioning all types of transdermal drug delivery to have a widespread impact on medicine.