Obtaining surgical care can be a troublesome task for patients in rural areas. Not only is quality care often hours away by car, but rural hospitals commonly face financial difficulties in recruiting and keeping surgeons on staff. However, a research team from Texas Tech University Health Sciences, Odessa, Texas, has developed a novel methodology to reduce rural area surgical costs, improve quality of care, and increase revenue for academic surgical programs. Their study findings were presented at the American College of Surgeons Clinical Congress 2017.
To address the challenges of rural surgery, the Texas Tech research team developed partnerships between rural hospitals and academic surgery departments so that each one can benefit from the other’s resources. To start, academic surgeons were placed in rural hospitals, which reduced the hospitals’ costs associated with recruiting and staffing surgeons. Since more rural hospitals had surgeons available on site, patient transfers were reduced. As a result of these partnerships, participating rural hospitals saw an average increase of $4.7 million in net revenue.
The partnerships also benefited the academic surgery departments. Because academic departments rely on Graduate Medical Education (GME) funding to offset the cost of indigent care and education, the partnerships have helped mitigate GME funding reductions.
Lead study author Saju Joseph, MD, FACS, stresses that one of the most important results of these partnerships was increased patient satisfaction. With patient transfers reduced by more than 70 percent in participating hospitals, Joseph and colleagues found that patients were substantially more satisfied with their local service. Patient survey results showed that on a scale of one to 10, average patient satisfaction jumped by an entire point due to the increased availability of surgical services.
“I’m a big believer that patients shouldn’t have to travel very far to get quality care, especially if it’s something that can be delivered close to home,” Joseph says.
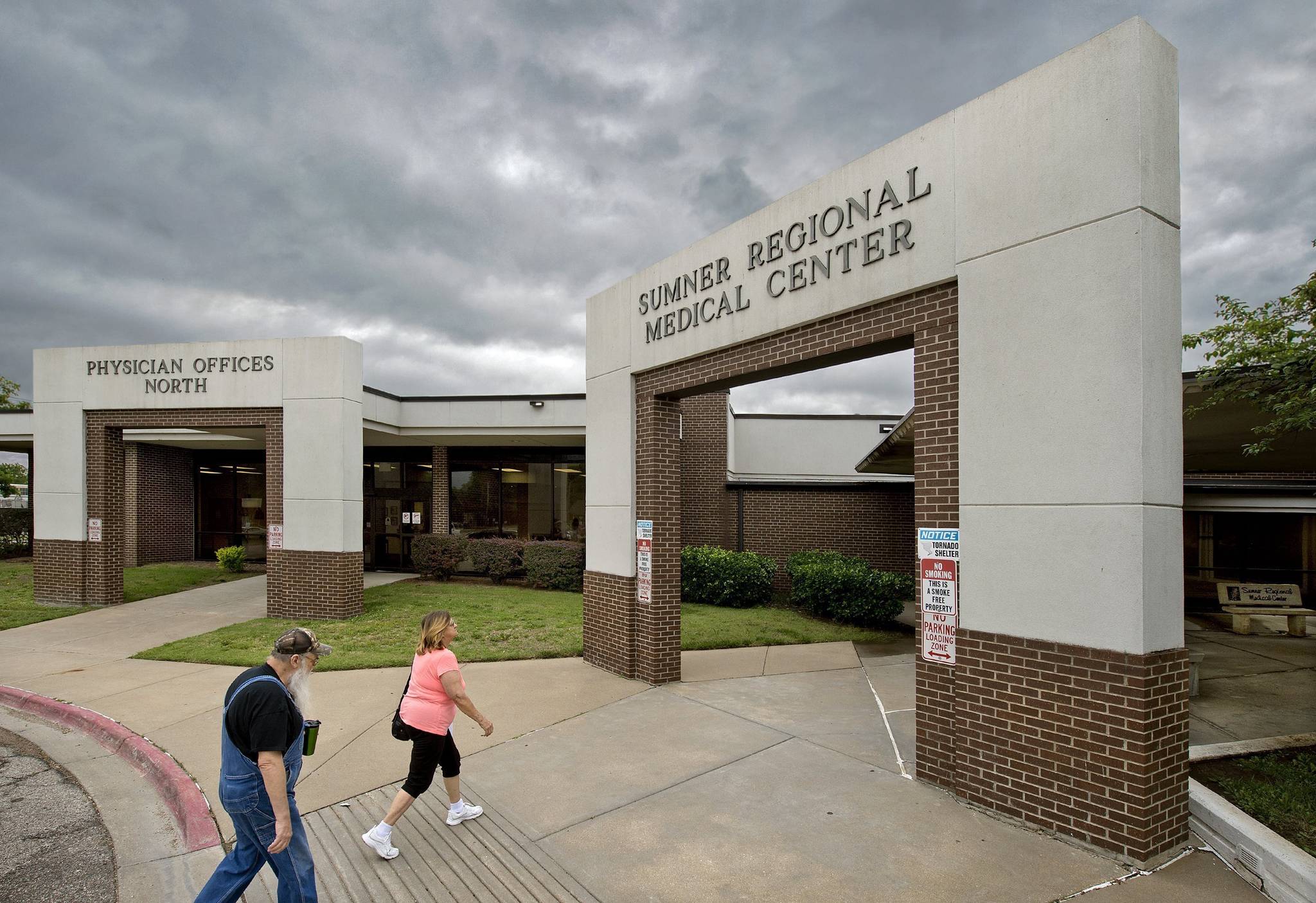
In this May 2017 photo people walk into the Sumner Regional Medical Center in Wellington, Kan. The center is facing the same financial troubles plaguing many rural hospitals. (Keith Myers/The Kansas City Star via AP)
With quality care more accessible through these partnerships, patients are able to receive care closer to home, allowing family members to visit more easily, a factor which contributed to patient satisfaction. Joseph said patients appreciated the outcomes, the quality of care, and, most importantly, the availability of surgical care.
The residents of the communities where these partnerships were developed were very aware of the effort to bring together academic surgeons and rural hospitals, according to Joseph. Announcements were distributed by local hospitals that they were partnering with academic institutions to bring surgeons into the community. For this pilot project, not only were surgical patients, rural hospitals, and academic institutions affected, but the counties benefitted as well.
“The way Texas works is unique because the counties pay for some patient transfers,” Joseph says. “For one small town, saving that money on transfers provided them money to pave their main road. These improvements really show the community that there is something positive going on.”
Due to these partnerships and the resulting decrease in transfers, the projected cost savings for the state of Texas is roughly $7 million, according to Joseph.
The research team was able to successfully develop partnerships for five hospitals. Joseph is confident that this model is not specific to rural surgery in West Texas, where the initial partnerships were set up, but is something that can benefit rural surgery in many different areas of the U.S.
“It’s a win-win situation for everybody,” Joseph says. “As, surgeons, we need to champion the idea of providing high quality care with low costs and providing a community benefit.”




