When an elderly person experiences a fall, it can lead to an array of very serious issues, from a broken bone to head trauma. As such, caregivers seek to reduce the chance for this incident to occur. Ultimately, not every situation or occurrence can be predicted or guarded against. One such time that can result in a fall is during a trip to the bathroom. Unfortunately, knowing when this need arises can be challenging for a caregiver, especially when the elderly person is in a care facility surrounded by many others who require the same level of treatment.
Seeking to address this problem, Simavita has developed a connected incontinence management system. Using a sensor device and software, the company offers a potential solution in an effort to reduce the chance of a fall occurring. Speaking on the development of this technology is the company’s CEO, Philippa Lewis, as well as the CTO, Peter Curran. In this interview, they discuss the challenges addressed during design, considerations that needed to be accounted for, connectivity and cloud implementation, and the next steps for the company.
Fenske: Thanks to both of you for speaking with me about your medical technology. First, can you please explain the relationship between falls and incontinence among the elderly?
Philippa Lewis: There are many white papers and studies that link an increase in falls in the elderly to urinary incontinence. In summary, patients that experience incontinence also have a high prevalence of urinary tract infections (UTIs). These residents still experience the urge to toilet themselves, but experience an increase in falls based on their mobility challenges and fragility. Caregivers in long-term care centers (LTCs) are not always readily available to toilet residents, and some of these residents experience dignity issues related to requiring help going to the bathroom.
Fenske: What does your technology solution do to address the problem?
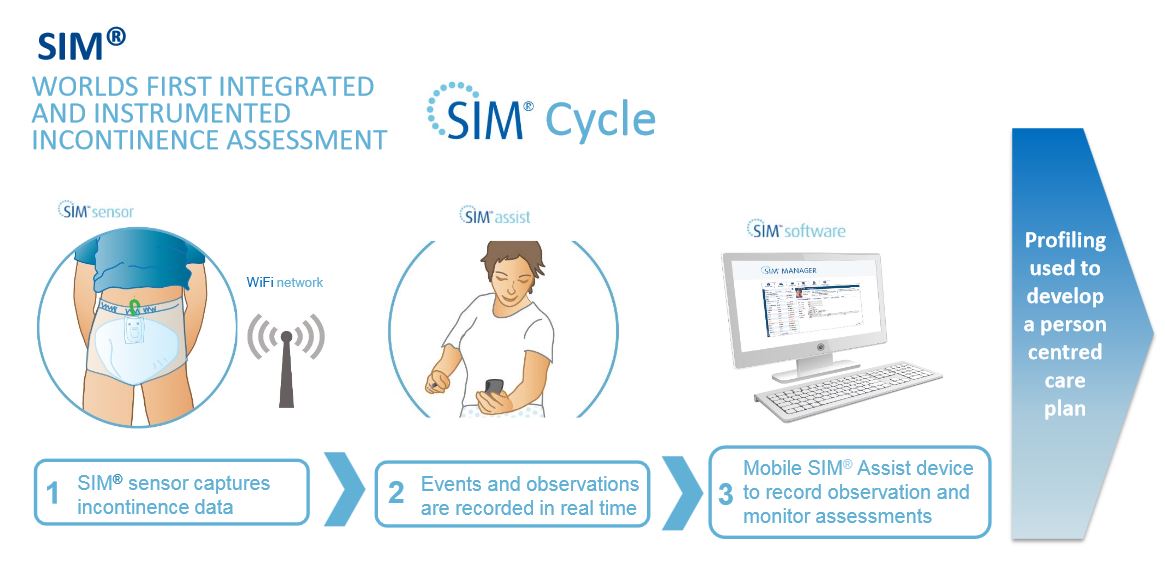
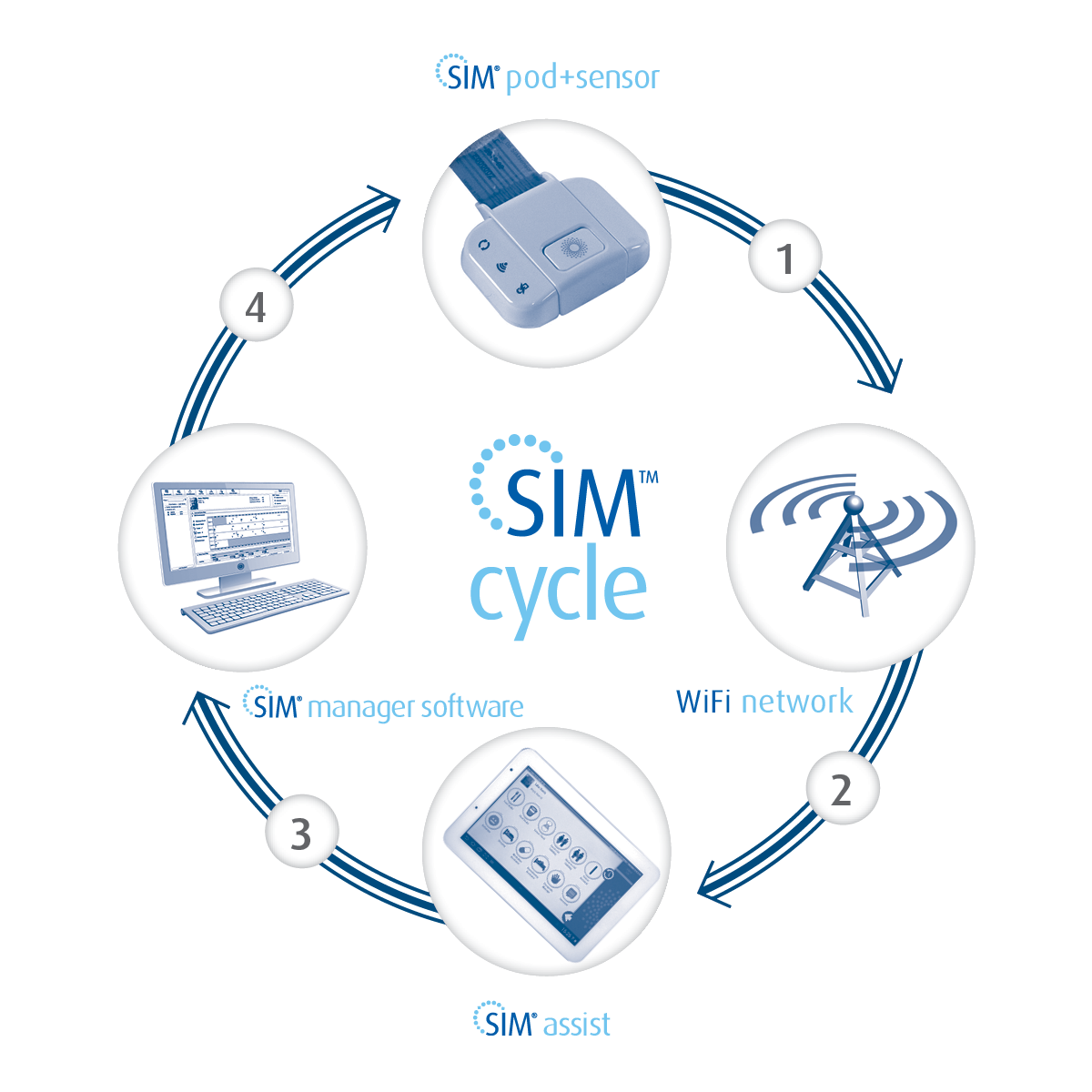
Lewis: SIM provides an evidence-based incontinence assessment that allows for toileting schedules in resident care plans to be developed based on the physiological needs of the resident. This evidence-based tool is different than the current practices of general toileting schedules (before and after meals, and before bedtime), which are common in most LTCs.
Peter Curran: Aligning toileting with physiological need increases the likelihood of productive toileting episodes, and correspondingly, reduces the likelihood of unplanned or unattended toileting episodes.
Fenske: What were the most significant challenges with developing your solution?
Lewis: Developing the software algorithms associated with interpreting the data detected by the sensor that allows for SIM to interpret and recommend proper toileting times. The actual sensor is very unique, as it can pick up multiple wetness events within the same diaper.
Curran: Detecting multiple wetness events and estimating associated volume in a diaper, especially with increasing wetness within the diaper, is complex and challenging. Diapers are non-uniform containers that are subjected to movement and pressure. Simavita’s solution combines sensor data with metaheuristic learning algorithms, refined by a significant amount of in-field testing.
Fenske: How was it managing the development of several unique pieces of the complete system?
Curran: Simavita has remained focused on delivering a complete assessment and care planning solution for incontinence. The product is a medical device, and therefore subject to a very significant regulatory framework; the SIM product has successfully gone through a full FDA clearance process. Developing and delivering medical devices requires strong discipline around product ideation – ideas and concepts through into proof of concept – and realization – development, manufacture, and delivery. So it has very much been about maintaining vision and focus, and ensuring resources, including all of our vital human capital, were aligned and have robust processes in place. We have also worked hard to identify and work with partners with global leadership in different aspects of our technology solutions; so we leverage great science and expertise globally.
Fenske: What considerations were there in the design of a wearable used by elderly patients?
Lewis: Comfort, toxicity, and compliance to the style and size. Understanding which diaper style to incorporate the sensor into. Where to place the pod, and how big it should be. Making sure we developed a product that people with dementia would be able to cope with. Designing the style and type of special over-pants with the pocket to hold the pod in place. Ensuring the pod design was user friendly.
Curran: In addition to those points, safety beyond toxicity (including safe management of electrical currents, flame retardant plastics, design for easy decontamination), battery life to ensure the product lasts for the full assessment duration between charges, and augmenting the user experience with smart point-of-care apps.
Fenske: What advantages does leveraging cloud technology offer to medical device manufacturers?
Lewis: Cloud-based technologies allow for medical device manufacturers to deploy and maintain their solutions without requiring their customers to purchase hardware such as servers and computers. The benefits to customers are many, but cost savings, related to not having to purchase servers and maintain hardware and software using their IT resources, are often quoted as the biggest benefit. All SIM software is hosted in the cloud in a HIPAA compliant SaaS (software as a service) model, which also allows for easy updating of new versions. Since SIM is hosted in the cloud, the customer is also not required to install software on PCs that will access our care planning software, as it can be accessed using an internet browser.
Fenske: How did you address connectivity with the technology? What solution did you use?
Lewis: Connectivity is a common question when deploying new technologies, and after extensive research related to LTCs, it was determined that flexibility was a key component to allow for our customers to access our SIM cloud. Wi-Fi is the most common and secure way to access and transmit data in the SaaS model in LTCs.
Curran: Wi-Fi offers great flexibility to leverage existing network assets and can be connected to many wide area network communication solutions (e.g., Wi-Fi to Ethernet, Wi-Fi to Cellular).
Fenske: Are you collecting the data from patients’ experiences with the device?
Lewis: The patient wears a sensor, which is imbedded in a diaper pad over the 72-hour incontinence assessment. Each time the patient has a voiding event, the sensor automatically detects the urine, and then transmits the data to our cloud-based SIM Manager software, where the leakage event is analyzed and graphed into a bowel and bladder chart that will be used for care planning at the end of the 72 hours. The bowel and bladder chart will show voiding (leakage) patterns during the 72 hour assessment, and from these patterns, an evidence-based toileting plan will be developed that allows for the caregiver to proactively toilet the patient before they have the urge to either leak into their incontinence product or try and toilet themselves (which can lead to falls).
Curran: We also make use of de-identified data (stripped of patient-specific information) to improve the algorithms used during the analysis process.
Fenske: Can this technology be transferred to address another medical condition (even with minor tweaking)?
Lewis: Yes, Simavita is currently evaluating other applications of this technology, but SIM was the first application launched using this technology.
Fenske: What’s on the horizon for the company?
Lewis: The company has the opportunity to develop, integrate, or invent new applications that can sit on the current platform. We are also working on an everyday sensor option that could go into any diaper. Plus, we are also keen to commercialize some diagnostic options for the sensor. Going into baby diapers is also a very real opportunity.
Curran: The evidence-based nature of what we do, combined with great software workflow, provides real opportunities in a range of areas to help people maintain their independence and dignity for as long as possible; it’s a win-win for people and those who care for them, for increasingly strained health budgets, and for medical professionals needing better insight for care management.
Watch the following video to see more about the SIM technology.