Learn about new and promising applications of energy-based medical systems and the challenges of developing them.
An engineer develops the pulsed waveform output for a PFA system. [Photo courtesy of Minnetronix Medical]
While modern medicine is awash in high-tech electronics — from large surgical robots to tiny implanted sensors — there are several applications where electrical energy is directly applied to a patient to ablate tissue, convey drugs, or achieve other clinical effects.
Given the obvious concerns with applying electricity to humans, developing these tools safely and effectively is crucial.
This article briefly reviews these applications of electrical energy in medicine. It also looks at new opportunities to refine existing technology such as radiofrequency (RF) ablation, or realize radical improvements using new energy modalities such as pulsed-field ablation (PFA).
Ablation
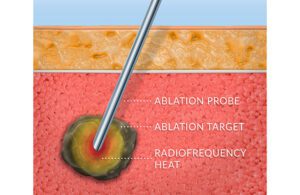
An ablation probe makes contact with a target, such as a tumor or nerve, and uses radiofrequency heat to kill diseased cells. [Illustration courtesy of Minnetronix]
RF is the most mature and prevalent technology, owing to its low cost, procedural simplicity, compatibility with minimally invasive techniques and well-understood performance. In RF ablation, high-frequency electrical current is conducted through an ablation target such as a tumor or nerve, causing heating and eventual cell death. The high frequency allows it to pass through tissue with minimal stimulation of muscle.
Modern RF ablation systems employ high-precision control systems which optimize ablation volume with minimal procedural time and can be tailored to specific clinical needs.
Pulsed-field ablation
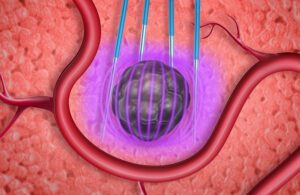
In pulsed-field ablation, electronic fields degrade cells to death in an irreversible process without heat. [Illustration courtesy of Minnetronix]
RELATED: Pulsed-field ablation enables new precision cancer treatments
PFA differs from RF in that it is tissue-selective, non-thermal and conducive to pre-planning:
- Tissue-selective: Different tissue types have markedly different susceptibility to the electric fields employed in PFA, and this can permit tissue type-selective ablation. Cardiac electrophysiology applications are benefiting from this selectivity by utilizing PFA to ablate cardiomyocytes (which are highly susceptible to PFA) while avoiding unwanted collateral damage to the nearby smooth muscle of the esophagus (which is poorly susceptible to PFA). This selectivity may potentially provide significant reduction in morbidity for prostate and pancreatic cancer compared to RF or other treatments.
- Non-thermal: While thermal ablation causes tissue necrosis and a subsequent inflammatory response, PFA causes cell death through apoptosis, which is the natural mechanism of cellular clearance and is not inflammatory. Patients thus benefit from quicker post-procedure recovery.
- Conducive to pre-planning: Thermal ablation is difficult to pre-plan, as thermal properties of tissue — “heat sinks” from nearby blood vessels, “insulators” from nearby structures, and non-homogeneity of the ablation target — vary so significantly as to make pre-planning difficult or intractable. The electric field-mediated mechanism of PFA, however, is affected by a smaller, less variable set of parameters, allowing for meaningful pre-planning and control of energy delivery. Future applications of PFA are likely to include a patient-specific energy prescription derived from pre-procedural imaging and therapy simulation.
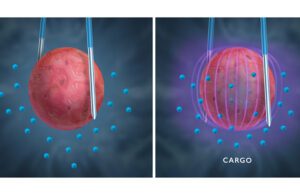
Pulsed-field ablation also uses electric pulses to trigger transient permeability of a cell to allow for drug delivery. This is a reversible process called electroporation. [Illustration courtesy of Minnetronix] [Illustration courtesy of Minnetronix]
Use of electroporation to deliver such a drug turns the device into a combination product, triggering higher levels of regulatory concerns and scrutiny. In development of such a system, most important is a clear understanding of the interaction between the tissue and electric field and the boundary between reversible electroporation, irreversible electroporation (pulsed-field ablation) and thermal ablation.
RELATED: In vivo electroporation is an engineering solution for drug and gene delivery
Developing an energy-based system

RF ablation and PFA circuitry [Photo courtesy of Minnetronix Medical]
Translating experience with RF systems to PFA systems
Despite similar foundational architecture between RF and PFA, achieving the desired clinical outcomes is not trivial and can require many iterations.
That said, experience in RF design provides a solid foundation for developing PFA systems. There are architectural similarities, as well as similarities in measuring clinical outputs that can be adapted. In setting out to develop a PFA system, having resources or partners with extensive RF experience can help limit pitfalls.
Design customization, avoiding platform entanglements

An engineer makes adjustments to a RF ablation system used for comparison testing.[Photo courtesy of Minnetronix Medical]
Being tied to a third-party platform can also entangle a developer in licensing agreements and hinders lifecycle planning. In a marketplace that will likely become as dynamic as any technology space in its early years, it behooves companies to develop their own capital systems for maximum flexibility expanding their portfolio.
Complete product lifecycle integration
It is surprising how many firms continue to plan development of complex systems like PFA programs in a piecemeal fashion. A typical system consists of several primary subsystems, each consisting of complex components and subassemblies.
A program of this magnitude needs to consider not just the immediate concerns of proof of concept to prototype, but how that prototype will translate through the process to commercialization.

Daniel Friedrichs [Photo courtesy of Minnetronix]
How to join the MDO Contributors Network
The opinions expressed in this blog post are the author’s only and do not necessarily reflect those of Medical Design & Outsourcing or its employees.




