Findings advance opportunities for a ‘pacemaker in a bottle’
Johns Hopkins heart researchers are unraveling the mystery of how a modified pacemaker used to treat many patients with heart failure, known as cardiac resynchronization therapy (CRT), is able to strengthen the heart muscle while making it beat in a coordinated fashion. In a new study conducted on animal heart cells described in the Journal of Clinical Investigation, the scientists show that CRT changes these cells so they can contract more forcefully. The researchers also identified an enzyme that mimics this effect of CRT without use of the device.
“These discoveries potentially give us new pathways to benefit more heart failure patients — not only those whose hearts beat out of sync, but also those who currently do not qualify for CRT therapy yet still need an effective treatment to help their heart pump stronger,” says David Kass, M.D., professor of medicine and biomedical engineering at the Johns Hopkins University School of Medicine and senior author of the study. “Understanding the inner workings of CRT at the biological level may lead, in essence, to a ‘pacemaker in a bottle.'”
The researchers say their ultimate goals are to develop drugs or genetic therapies that strengthen failing hearts and to design a test to identify patients who would be most likely to benefit from CRT.
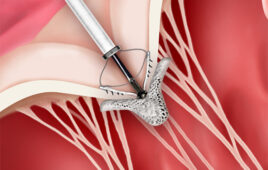
Kass explains that while the typical implanted pacemaker has only one wire that stimulates the right side of the heart, the CRT pacemaker has two wires. The second wire goes to the surface of the left side of the heart to enable both sides of the heart to be stimulated together.
CRT helps people whose hearts beat out of sync — one side is activated to “beat” before the other, preventing the muscle from pumping blood evenly. This condition is known as dyssynchrony. CRT “paces” the rhythms of both sides to restore a coordinated beat.
In their experiments, the researchers used an animal model of heart failure with dyssynchrony and also examined the impact of CRT on the heart. By studying isolated muscle tissue and muscle cells, they examined the relationship between contraction and the calcium that triggers it. In the hearts that beat out of sync, force from the muscle cells and the level of calcium needed to generate contractions were very much reduced. CRT improved contraction force more than calcium, and this led to the discovery that CRT had increased the sensitivity of the muscle to calcium.
The next question was how this change had occurred. Calcium sensitivity is a property of the proteins that form the contracting “engine” of muscle, so the investigators examined how these proteins had been biochemically altered by CRT. After ruling out all the known ways this might have occurred, they turned to a newer approach, testing for changes in more than 150 proteins and discovered that CRT specifically modified 13 of them.
“Once we discovered which proteins were being altered, we were able to identify an enzyme likely responsible for these changes,” noted lead author Jonathan Kirk, Ph.D., a post-doctoral fellow at the Johns Hopkins University School of Medicine. Working with heart muscle and isolated cells from the same animal models, the researchers found that the enzyme turned out to be GSK-3 beta, which was able to convert the behavior of muscle cells from a heart that was beating out of sync to what looked like heart cells that had received CRT, essentially mimicking the effect of CRT.
In further lab experiments, Kass and his colleagues found that although GSK-3 beta was inactive in muscle from a failing and dyssynchronous heart, it was reactivated by CRT. When that happened, the enzyme altered the motor proteins so that they generated greater force using the same amount of calcium-based activation.
“It had never been shown before that GSK-3 beta could modify motor proteins in the heart to make them more sensitive to calcium. It is surprising that this same type of effect can be produced by a pacemaker therapy like CRT,” says Kass.
Nearly all existing medications for heart failure increase heart contraction by enhancing levels of calcium available to muscle cells, but over time, these higher levels can be toxic to the heart.
Altering the calcium sensitivity of the muscle is not the only way CRT can improve heart function. In a study published in 2011, Kass and colleagues also showed that CRT enables heart muscle to respond to hormones, such as adrenaline, which stimulates pumping ability, in a similar way to what happens during exercise.
The Kass Lab played a key role in developing CRT for use in patients in the late 1990s. The Food and Drug Administration approved CRT in 2001, and it is widely used today to improve symptoms and help people live longer.
In an unusual twist to the way therapies are usually developed, CRT was first tested in patients, but the biological mechanisms as to why it worked were not understood. The new work is running the discovery clock backwards, revealing these mechanisms and their potential to benefit many patients with heart failure.
For more information, visit Johns Hopkins Medicine.