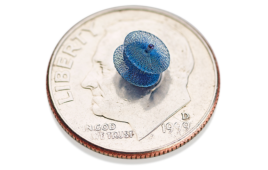
The dissolvable, transient pacemaker is flexible, elastic and wireless. [Image courtesy of Northwestern University]
The team designed a transient pacemaker — one of the world’s first — last year. The fully implantable, wireless device dissolves in the body after it is no longer needed. The new smart pacemaker features a coordinated network of soft, flexible, wireless, wearable sensors and control units outside of the body that can communicate with each other.
“This marks the first time we have paired soft, wearable electronics with transient electronic platforms,” John Rogers, one of the lead researchers on the project, said in a news release. “This approach could change the way patients receive care providing multimodal, closed-loop control over essential physiological processes — through a wireless network of sensors and stimulators that operates in a manner inspired by the complex, biological feedback loops that control behaviors in living organisms.”
Algorithms in the smart pacemaker analyze physiological functions, including body temperature, oxygen levels, respiration, muscle tone, physical activity and heart electrical activity, to autonomously detect abnormal cardiac rhythms. The pacemaker can then decide when to pace the heart and at what rate.
All information from the smart pacemaker can be sent to a smartphone or tablet for physicians to remotely monitor patients.
The pacemaker system is designed to eliminate the need for external hardware, including wires or leads, as it harvests energy from a small, wireless device that softly adheres to a patient’s chest.
The researchers suggest the device could be used in patients who need temporary pacing after cardiac surgery or those who are waiting for a permanent pacemaker.
“For temporary cardiac pacing, the system untethers patients from monitoring and stimulation apparatuses that keep them confined to a hospital setting. Instead, patients could recover in the comfort of their own homes while maintaining the peace of mind that comes with being remotely monitored by their physicians,” said Rogers, who is also a professor of materials science and engineering, biomedical engineering and neurological surgery at Northwestern’s McCormick School of Engineering and Northwestern University Feinberg School of Medicine. “This also would reduce the cost of health care and free up hospital beds for other patients.”
Rogers and the research team designed the pacemaker using four different skin-interfaced devices coordinated with their existing bioresorbable, leadless pacemaker. The soft, flexible device is mounted on the skin and can be gently peeled off after use. The pacemaker naturally dissolves in the body when it is no longer needed.
The system has a body-area network that consists of a battery-free, transient, bioresorbable pacemaker; a cardiac module that sits on the chest to provide power to and control stimulation parameters; a hemodynamics module that sits on the forehead to sense pulse oximetry, tissue oxygenation and vascular tone; a respiratory module at the base of the throat to monitor coughing and respiratory activity; and a multi-haptic feedback module that vibrates and pulses to communicate with a patient.
“We wanted to demonstrate that it’s possible to deploy multiple different types of devices, each performing essential functions in a wirelessly coordinated manner across the body,” Rogers said. “Some are sensing. Some are delivering power. Some are stimulating. Some are providing control signals. But they all work together, trading information, making decisions based on algorithms and reacting to changing conditions. The vision of multiple bioelectronic devices all talking to one another and performing different functions at different relevant anatomical locations is a frontier area that we will continue to pursue going into the future.”
The researchers suggest the device could also be beneficial for vulnerable patients, most notably babies who are born with a hole in the wall that separates the heart’s upper chambers.
“The good news is this is a temporary condition,” said Igor Efimov, a professor of biomedical engineering in McCormick and professor of medicine (cardiology) in Feinberg. “After about five to seven days, the heart regains its ability to stimulate itself and no longer needs a pacemaker. The procedure to remove the pacemaker has improved greatly over the years, so the rate of complications is low. But we could free these babies from the wires connecting to an external generator and free them from needing a second procedure.”
The study was published in the journal Science and was led by Rogers, Efimov and Rishi Arora, who is a professor of medicine at Feinberg and co-director of the Center for Arrhythmia Research.