New Alzheimer’s biomarker results reported at Alzheimer’s Association International Conference 2014
A decreased ability to identify odors might indicate the development of cognitive impairment and Alzheimer’s disease, while examinations of the eye could indicate the build-up of beta-amyloid, a protein associated with Alzheimer’s, in the brain, according to the results of four research trials reported today at the Alzheimer’s Association International Conference 2014 (AAIC 2014) in Copenhagen.
In two of the studies, the decreased ability to identify odors was significantly associated with loss of brain cell function and progression to Alzheimer’s disease. In two other studies, the level of beta-amyloid detected in the eye (a) was significantly correlated with the burden of beta-amyloid in the brain and (b) allowed researchers to accurately identify the people with Alzheimer’s in the studies.
Beta-amyloid protein is the primary material found in the sticky brain “plaques” characteristic of Alzheimer’s disease. It is known to build up in the brain many years before typical Alzheimer’s symptoms of memory loss and other cognitive problems.
“In the face of the growing worldwide Alzheimer’s disease epidemic, there is a pressing need for simple, less invasive diagnostic tests that will identify the risk of Alzheimer’s much earlier in the disease process,” said Heather Snyder, Ph.D., Alzheimer’s Association director of Medical and Scientific Operations. “This is especially true as Alzheimer’s researchers move treatment and prevention trials earlier in the course of the disease.”
“More research is needed in the very promising area of Alzheimer’s biomarkers because early detection is essential for early intervention and prevention, when new treatments become available. For now, these four studies reported at AAIC point to possible methods of early detection in a research setting to choose study populations for clinical trials of Alzheimer’s treatments and preventions,” Snyder said.
With the support of the Alzheimer’s Association and the Alzheimer’s community, the United States created its first National Plan to Address Alzheimer’s Disease in 2012. The plan includes the critical goal, which was adopted by the G8 at the Dementia Summit in 2013, of preventing and effectively treating Alzheimer’s by 2025. It is only through strong implementation and adequate funding of the plan, including an additional $200 million in fiscal year 2015 for Alzheimer’s research, that we’ll meet that goal.
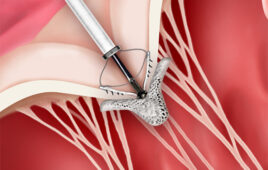
Clinically, at this time it is only possible to detect Alzheimer’s late in its development, when significant brain damage has already occurred. Biological markers of Alzheimer’s disease may be able to detect it at an earlier stage. For example, using brain PET imaging in conjunction with a specialized chemical that binds to beta-amyloid protein, the buildup of the protein as plaques in the brain can be revealed years before symptoms appear. These scans can be expensive and are not available everywhere. Amyloid can also be detected in cerebrospinal fluid through a lumbar puncture where a needle is inserted between two bones (vertebrae) in your lower back to remove a sample of the fluid that surrounds your brain and spinal cord.
Greater Neurodegeneration Associated with Worse Olfactory Function in Cognitively Normal Elderly
There is growing evidence that the decreased ability to correctly identify odors is a predictor of cognitive impairment and an early clinical feature of Alzheimer’s. As the disease begins to kill brain cells, this often includes cells that are important to the sense of smell.
Matthew E. Growdon, B.A., M.D./M.P.H. candidate at Harvard Medical School and Harvard School of Public Health, and colleagues investigated the associations between sense of smell, memory performance, biomarkers of loss of brain cell function, and amyloid deposition in 215 clinically normal elderly individuals enrolled in the Harvard Aging Brain Study at the Massachusetts General Hospital. The researchers administered the 40-item University of Pennsylvania Smell Identification Test (UPSIT) and a comprehensive battery of cognitive tests. They also measured the size of two brain structures deep in the temporal lobes – the entorhinal cortex and the hippocampus (which are important for memory) – and amyloid deposits in the brain.
At AAIC 2014, Growdon reported that, in this study population, a smaller hippocampus and a thinner entorhinal cortex were associated with worse smell identification and worse memory. The scientists also found that, in a subgroup of study participants with elevated levels of amyloid in their brain, greater brain cell death, as indicated by a thinner entorhinal cortex, was significantly associated with worse olfactory function – after adjusting for variables including age, gender, and an estimate of cognitive reserve.
“Our research suggests that there may be a role for smell identification testing in clinically normal, older individuals who are at risk for Alzheimer’s disease,” said Growdon. “For example, it may prove useful to identify proper candidates for more expensive or invasive tests. Our findings are promising but must be interpreted with caution. These results reflect a snapshot in time; research conducted over time will give us a better idea of the utility of olfactory testing for early detection of Alzheimer’s.”
The Harvard Aging Brain Study is funded by the U.S. National Institute on Aging and the Alzheimer’s Association.
Odor Identification Deficits Linked with Transition from Mild Cognitive Impairment to Alzheimer’s
Davangere Devanand, M.B.B.S., M.D., Professor of Psychiatry (in Neurology and in the Sergievsky Center) at Columbia University Medical Center and colleagues investigated a multi-ethnic (34% White, 30% African-American, 36% Hispanic) sample of 1037 non-demented elderly people in New York City, with an average age of 80.7, and assessed them in a variety of ways at three time periods – from 2004-2006, 2006-2008, and 2008-2010. UPSIT was administered in English and Spanish between 2004 and 2006. During follow-up 109 people transitioned to dementia (101=Alzheimer’s); there were 270 deaths.
At AAIC 2014, Devanand reported that, in 757 subjects who were followed, lower odor identification scores on UPSIT were significantly associated with the transition to dementia and Alzheimer’s disease, after controlling for demographic, cognitive, and functional measures, language of administration, and apolipoprotein E genotype. For each point lower that a person scored on the UPSIT, the risk of Alzheimer’s increased by about 10%. Further, lower baseline UPSIT scores, but not measures of verbal memory, were significantly associated with cognitive decline in participants without baseline cognitive impairment.
“Odor identification deficits were associated with the transition to dementia and Alzheimer’s disease, and with cognitive decline in cognitively intact participants, in our community sample. The test was effective in both English and Spanish,” said Devanand. “If further large-scale studies reproduce these results, a relatively inexpensive test such as odor identification may be able to identify subjects at increased risk of dementia and Alzheimer’s disease at a very early stage, and may be useful in identifying people at increased risk of cognitive decline more broadly.”
Eye Exam for Beta-Amyloid Correlates with Levels in the Brain and Detects People with Alzheimer’s
Recent studies have identified beta-amyloid plaques in the retinas of people with Alzheimer’s – similar to those found in the brain – suggesting the possibility of simple, non-invasive methods of early detection.
At AAIC 2014, Shaun Frost of the CSIRO (Commonwealth Scientific and Industrial Research Organization, Australia) and colleagues reported preliminary results of a study of volunteers who took a proprietary supplement containing curcumin, which binds to beta-amyloid with high affinity and has fluorescent properties that allow amyloid plaques to be detected in the eye using a novel system from NeuroVision Imaging, LLC, and a technique called retinal amyloid imaging (RAI). Volunteers also underwent brain amyloid PET imaging to correlate the retina and brain amyloid accumulation.
An abstract prepared by the scientists for AAIC 2014 gives the results for 40 participants out of 200 total in the study. The full study is expected to be completed later this year.
Preliminary results suggest that amyloid levels detected in the retina were significantly correlated with brain amyloid levels as shown by PET imaging. The retinal amyloid test also differentiated between Alzheimer’s and non-Alzheimer’s subjects with 100 percent sensitivity and 80.6 percent specificity.
Furthermore, longitudinal studies on an initial cohort demonstrated an average of 3.5% increase in retinal amyloid over a 3.5-month period of time demonstrating promise of the technique as a means for monitoring response to therapy.
“We envision this technology potentially as an initial screen that could complement what is currently used: brain PET imaging, MRI imaging, and clinical tests,” Frost said. “If further research shows that our initial findings are correct, it could potentially be delivered as part of an individual’s regular eye check-up. The high resolution level of our images could also allow accurate monitoring of individual retinal plaques as a possible method to follow progression and response to therapy.”
The trial is a collaboration between CSIRO, Edith Cowan University, McCusker Alzheimer’s Research Foundation and California-based NeuroVision Imaging. The project is part of the Australian Imaging and Biomarkers Lifestyle Study of Aging (AIBL).
Amyloid Detected in the Lens of the Eye Strongly Correlates to Amyloid Levels Detected in the Brain
At AAIC 2014, Paul D. Hartung, M.S, President and CEO of Cognoptix, Inc. and colleagues reported the results of a study of a novel fluorescent ligand eye scanning (FLES) system that detects beta-amyloid in the lens of the eye using a topically-applied ointment that binds to amyloid and a laser scanner.
The researchers studied 20 people with probable Alzheimer’s disease, including mild cases, and 20 age-matched healthy volunteers; all participants’ Alzheimer’s status was masked from the observers. The ointment was applied to the inside of participants’ lower eyelids the day before measurement. Laser scanning detected beta-amyloid in the eye by the presence of a specific fluorescent signature. Brain amyloid positron emission tomography (PET) scanning was performed on all participants to estimate amyloid plaque density in the brain.
Using results from the fluorescent imaging, researchers were able to differentiate people with Alzheimer’s from healthy controls with high sensitivity (85 percent) and specificity (95 percent). In addition, amyloid levels based on the eye lens test correlated significantly with results obtained through PET brain imaging. No serious adverse events were reported, according to the scientists.
“There is a critical need for a fast, dependable, low-cost and readily available test for the early diagnosis and management of Alzheimer’s disease,” said Pierre N. Tariot, M.D., Director of the Banner Alzheimer’s Institute in Phoenix, and a principal investigator in the study.
“The results of this small Phase 2 feasibility study validate our previously reported results and demonstrate the ability of the FLES system to reproduce the findings of clinical diagnosis of Alzheimer’s with high sensitivity and specificity,” said Hartung. “This system shows promise as a technique for early detection and monitoring of the disease.”