Using skin-derived stem cells (SDSCs) and a previously developed collagen tube designed to successfully bridge gaps in injured nerves in rat models, the research team in Milan, Italy that established and tested the procedure has successfully rescued peripheral nerves in the upper arms of a patient suffering peripheral nerve damage who would have otherwise had to undergo amputations.
The study will be published in a future issue of Cell Transplantation but is currently freely available on-line as an unedited early e-pub at: http://www.ingentaconnect.com/content/cog/ct/pre-prints/content-ct1096.
“Peripheral nerve repair with satisfactory functional recovery remains a great surgical challenge, especially for severe nerve injuries resulting in extended nerve defects,” said study corresponding author Dr. Yvan Torrente, of the Department of Pathophysiology and Transplantation at the University of Milan. “However, we hypothesized that the combination of autologous (self-donated) SDSCs placed in collagen tubes to bridge gaps in the damaged nerves would restore the continuity of injured nerves and save from amputation the upper arms of a patient with poly-injury to motor and sensory nerves.”
Although autologous nerve grafting has been the ‘gold standard’ for reconstructive surgeries, these researchers felt that there were several drawbacks to that approach, including graft availability, donor site morbidity, and neuropathic pain.
According to the researchers, autologous SDSCs have advantages over other stem cells as they are an accessible source of stem cells rapidly expandable in culture, and capable of survival and integration within host tissues.
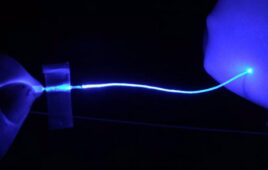
While the technique of using the collagen tubes – NeuraGen, an FDA-approved device – to guide the transplanted cells over gaps in the injured nerve had been previously developed and tested by the same researchers with the original research successfully saving damaged sciatic nerves on rats, the present case, utilizing the procedure they developed employing SDSCs and a nerve guide, is the first to be carried out on a human.
Over three years, the researchers followed up on the patient, assessing functional recovery of injured median and ulnar nerves by pinch gauge test and static two-point discrimination and touch test with monofiliments along with electrophysiological and MRI examinations.
“Our three-year follow up has witnessed nerve regeneration with suitable functional recovery in the patient and the salvage of upper arms from amputation,” said the researchers. “This finding opens an alternative avenue for patients who are at-risk of amputation after the injury to important nerves.”
“This single case study provides the first step towards a proof-of-principle for a new treatment for peripheral nerve injury,” said Dr. Camillo Ricordi, coeditor-in-chief of Cell Transplantation, Stacy Joy Goodman Professor of Surgery and Director of the Cell Transplant Center at the University of Miami. “Further studies will be necessary to determine whether the work in this report could be validated, introducing a novel therapeutic strategy for peripheral nerve injury.”