A new study suggests that healthcare professionals (HCPs) should heed to their own advice: stay home when sick.
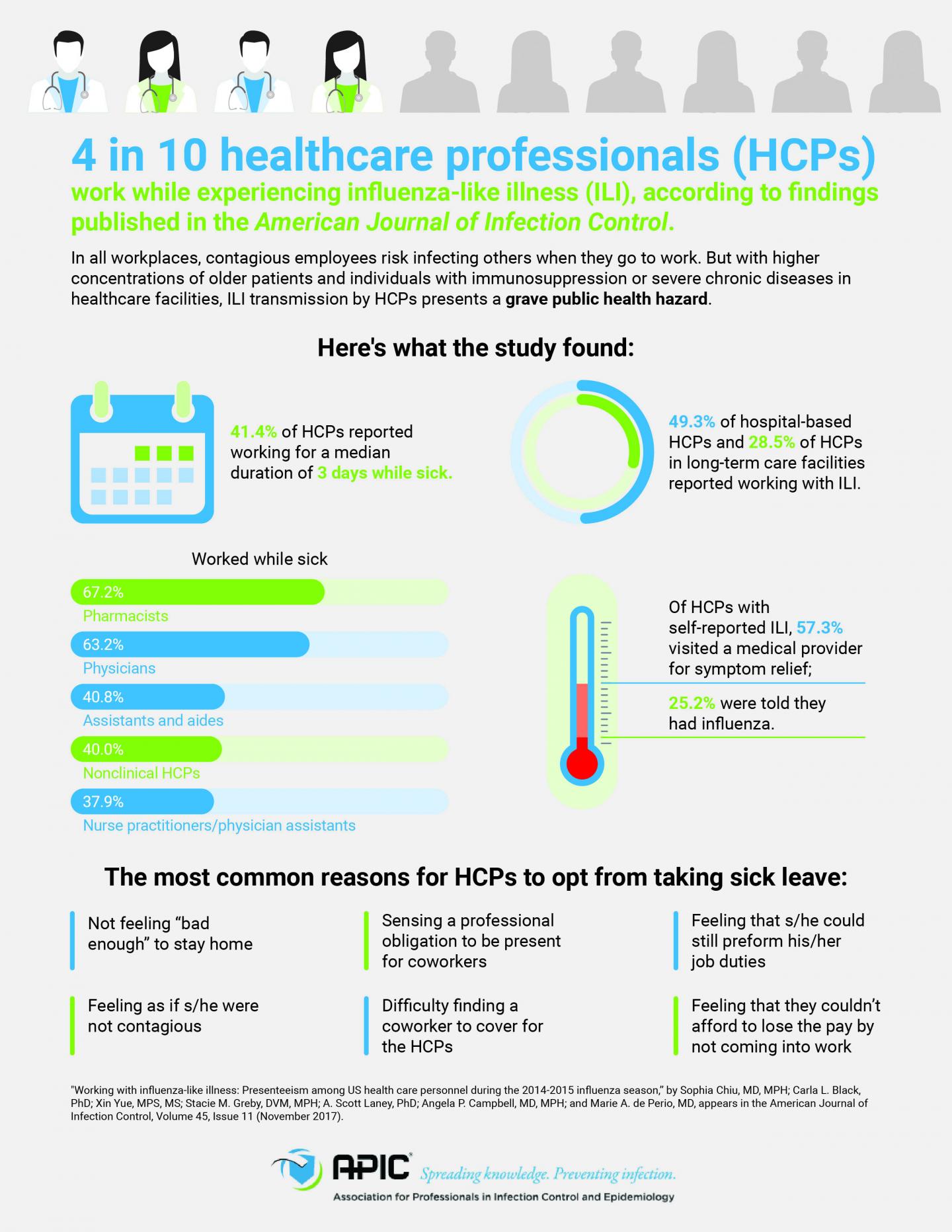
Some four in 10 HCPs work while experiencing influenza-like illness (ILI), according to findings published in the November issue of the American Journal of Infection Control (AJIC), the journal of the Association for Professionals in Infection Control and Epidemiology (APIC). As in all workplaces, contagious employees risk infecting others when they turn up for work. But with higher concentrations of older patients and individuals with immunosuppression or severe chronic diseases in healthcare facilities, ILI transmission by HCPs presents a grave public health hazard.

“The statistics are alarming. At least one earlier study has shown that patients who are exposed to a healthcare worker who is sick are five times more likely to get a healthcare-associated infection,” says lead researcher Sophia Chiu, MD, MPH, CDC’s National Institute for Occupational Safety and Health. “We recommend all healthcare facilities take steps to support and encourage their staff to not work while they are sick.”
The annual study, conducted via a national online survey, collected data from from 1,914 HCPs during the 2014-2015 influenza season. Respondents self-reported ILI, defined as the combination of a fever and cough or sore throat, and listed factors that prompted them to turn up for work.
The survey assessed a variety of health occupations across multiple institutions: physicians; nurse practitioners and physician assistants; nurses; pharmacists; assistants/aides; other clinical HCP; nonclinical HCPs; and students. Four types of work settings were assessed: hospitals; ambulatory care or physician offices; long-term care facilities; or other clinical settings.
Among the findings:
- Of the 1,914 HCPs surveyed, 414 reported ILI. Of these, 183–or 41.4 percent–reported working for a median duration of three days while experiencing influenza-like symptoms.
- Hospital-based HCPs had the highest frequency of working with ILI (49.3 percent), compared to HCPs at long-term care facilities (28.5 percent). Clinical professional HCPs were the most likely to work with ILI (44.3 percent), with pharmacists (67.2 percent) and physicians (63.2 percent) among those with the highest frequency.
- In contrast, the survey found that assistants and aides (40.8 percent), nonclinical HCPs (40.4 percent), nurse practitioners/physician assistants (37.9 percent), and other clinical HCPs (32.1 percent) worked while sick.
- The most common reasons for HCPs to opt from taking sick leave included feeling that s/he could still preform his/her job duties; not feeling “bad enough” to stay home; feeling as if s/he were not contagious; sensing a professional obligation to be present for coworkers; and difficulty finding a coworker to cover for him/her. Among the HCPs who felt they could still preform their job duties, 39.0 percent sought medical attention for their ILI symptoms, as did 54.0 percent of those who did not think they were contagious. 49.8 percent of HCPs in long-term care settings who reported for work when sick reported doing so because they couldn’t afford to lose the pay.
- Previously published results from this survey described that only 77.3 percent of respondents reported receiving a flu shot. The U.S. Department of Health and Human Services’ Healthy People 2020 aims to reach a 90 percent influenza vaccination rate for HCPs.
- HCPs with self-reported ILI missed a median number of two work days. Of this cohort, 57.3 percent visited a medical provider for symptom relief; 25.2 percent were told they had influenza. The Centers for Disease Control and Prevention recommends that anyone with ILI wait 24-hours after a fever breaks before returning to work.
“Patients’ health and wellbeing are at stake when contagious HCPs opt not to stay home. Tailored strategies per occupation and health institution, including updating paid sick leave policies, can empower HCPs to make healthy choices not only for themselves, but for their coworkers and patients,” says Linda Greene, RN, MPS, CIC, FAPIC, 2017 APIC president.
From 1976-2007, influenza-associated fatalities accounted for up to 16.7 (ranged between 1.4 and 16.7) deaths per 100,000 people in the U.S. Flu-related deaths predominantly impact individuals 65 years and older. Influenza may be transmissible from one day before, and up to seven days after, symptoms onset.




