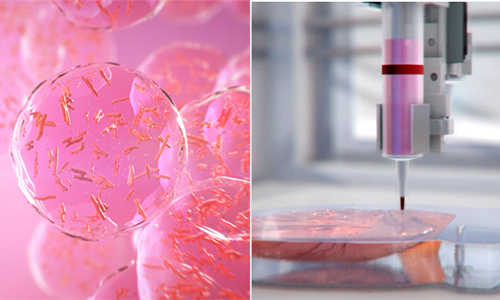
Researchers at the Saban Research Institute of Children’s Hospital in Los Angeles generated mouse and human tissue-engineered livers from organoid units composed of stem and progenitor cells, according to a study published in Stem Cells Translational Medicine last month.
Researchers at the Saban Research Institute of Children’s Hospital in Los Angeles generated mouse and human tissue-engineered livers from organoid units composed of stem and progenitor cells, according to a study published in Stem Cells Translational Medicine last month.
The tissue-engineered liver demonstrated normal attributes such as hepatocytes and blood cells and even restored some liver function in a mouse model of liver failure, according to the study.
Even though liver disease is common among Americans, researchers have not come up with an effective therapy that doesn’t include transplantation. Liver transplants are scarce and require a lifelong regimen of daily immunosuppressant medications.
“Based on the success in my lab generating tissue-engineered intestine and other cell types, we hypothesized that by modifying the protocol used to generate intestine, we would be able to develop liver organoid units that could generate functional tissue-engineered liver when transplanted,” pediatric surgeon and co-principal investigator Dr. Tracy Grikscheit said in prepared remarks.
The team grew liver organoid units from a heterogeneous mix of adult stem and progenitor cells. The units were implanted into mice models, which grew into tissue-engineered livers. Studies of the functionality of the resulting tissue showed that it had key components such as endothelial cells and blood vessels, but that the cellular organization was different from native liver tissue.
“A cellular therapy for liver disease would be a game-changer for many patients, particularly children with metabolic disorders,” noted pediatric surgeon and co-principal investigator Dr. Kasper Wang. “By demonstrating the ability to generate hepatocytes comparable to those in native liver, and to show that these cells are functional and proliferative, we’ve moved one step closer to that goal.”