Patient monitoring device connectors will need to be more compact, more durable, and able to handle higher data rates.
Patient monitoring device connectors will need to be more compact, more durable, and able to handle higher data rates.
By Rick Lopez, Paul Pulkowski and Jana Wagner, binder
By 2050, the number of people aged 60 or older is expected to double to 2 billion worldwide. During the same period, the number of persons aged 80 and older is predicted to triple to about 430 million.
This demographic shift is already creating higher demand for a wide range of medical equipment and services. The growing number of chronically ill patients in Western society will further increase the need for medical technology in the coming decades. An alarming 70% of deaths worldwide are caused by noncommunicable diseases such as heart failure, diabetes, and cancer. Because these are chronic conditions, patients and healthcare providers regularly monitor changes in indicators such as glucose levels and blood pressure.
Patient monitoring refers to observing, tracking, and analyzing a patient’s health and relaying that information to and between healthcare providers. In real-time, monitoring devices can detect deviations from baseline health parameters and notify healthcare providers when intervention may be necessary. On an ongoing basis, data from these devices helps medical professionals analyze patterns and detect early signs of deterioration or other developments. Patient monitoring is primarily used in clinical settings, including intensive care units, operating rooms, and post-anesthesia care units. However, recent innovations enable remote monitoring, allowing patients to remain at home or in other non-clinical settings while staying connected to healthcare providers.
Components of patient monitoring systems

MDO contributor Jana Wagner is a product manager at binder, responsible for medical-grade connectors and other customer-specific projects.
Patient monitoring equipment relies on several key components. Sensors play a crucial role in measuring physiological parameters such as body temperature, blood pressure, and oxygen saturation. Connectivity is required to transmit data and analysis to a monitoring station or other medical devices. This allows healthcare professionals to review the collected data on-site or remotely.
Patient monitoring systems also require enough server capacity to store electronic medical records so this data can be shared between physicians, facilities, and patients. Monitoring devices include alarm systems, which are triggered when predefined values are detected. For example, a pacemaker may alert a caregiver when a patient’s heart rate reaches a certain level. These features enable healthcare providers to intervene quickly. Advanced patient monitoring systems incorporate trend analysis and other decision-support tools to help clinicians make treatment decisions.
Patient monitoring devices must meet extensive regulatory requirements to be approved for medical use. These include:
- Accuracy: Equipment must be precise enough to detect even minute changes in a patient’s condition.
- Reliability: A failure of function or connectivity can adversely impact patient care, making durability a crucial requirement for every component of a device.
- Connectivity: Connecting to electronic health records (EHRs) and other medical devices can help streamline patient monitoring and improve patient outcomes.
- Ease of use: Healthcare equipment should be easy to use, with intuitive controls and minimal setup required so a person without medical training can operate a device if needed.
- Portability: Portable monitoring equipment is useful for monitoring patients in different settings, including hospitals, clinics, and homes, as well as in emergency vehicles.
- Alarms and alerts: Patient monitoring equipment can be programmed to alert healthcare providers to relevant changes in a patient’s condition.
- Data analysis: Patient data should provide healthcare providers with insights that support treatment decisions.
- Security: Wireless networks used in patient monitoring applications require the highest levels of security to protect patient data and privacy.
Critical requirements for medical-grade connectors in patient monitoring

MDO contributor Paul Pulkowski is a marketing manager at binder USA and a specialist for circular connectors.
Connectivity is crucial in transferring data in real-time or at periodic sequences between medical devices and providers. Medical-grade connectors must be designed for compatibility with specific devices and equipment, ensuring proper electrical and mechanical connections.
Standardization of connector types helps promote interoperability across different manufacturers and devices. Medical-grade connectors should adhere to stringent safety standards and regulations, such as IEC 60601-1, ensuring electrical safety, insulation, and grounding. Shock vibration (DIN EN 60601-1-11) and rough handling (DIN EN 60601-1) are especially important for use in portable equipment. Medical-grade connectors should also incorporate features like locking mechanisms or color-coded coding to prevent accidental disconnections or mismating.
Medical-grade connectors must meet industry standards and regulations, such as ISO 13485, which applies to quality management systems and specific standards related to electrical safety and medical devices. Compliance with these standards ensures that connectors are manufactured and tested according to recognized best practices. Another important international standardization is ISO 10993-5, which certifies biocompatibility in medical-grade connectors. Biocompatiblity plays a crucial role in ensuring that the material cannot cause harm to living cells.
Medical-grade connectors in patient monitoring devices need to be reliable and robust, capable of withstanding frequent use, repeated connections, and disconnections without compromising signal integrity. They should also be resistant to environmental factors like dust, moisture, and physical stress to ensure consistent and accurate data transmission.
Regarding durability, medical-grade connectors should be able to withstand the demands of healthcare settings. They should be resistant to wear and tear, chemical exposure, and frequent cleaning and high-temperature disinfection procedures, ensuring a long lifespan and reducing the need for frequent replacements. At the same time, medical-grade connectors must be easy to use. They should be designed for intuitive connection, disconnection, and handling. Features like ergonomic grip, tactile feedback, and clear markings or indicators help healthcare professionals to quickly and correctly connect the devices, reducing the risk of errors or delays.
These considerations are essential to ensuring seamless and reliable data transmission, patient safety, and interoperability with existing medical equipment.
Connectivity and patient monitoring

MDO contributor Rick Lopez is a senior sales engineer and project manager at binder group subsidiary binder USA.
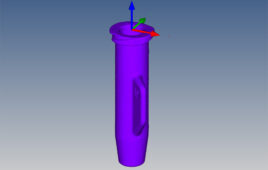
For the connectivity aspect of patient monitoring, key trends are advances in materials, miniaturization of components, and increased signal transmission capabilities. Consequently, connectors will need to be more compact, more durable, and handle higher data rates allowing medical devices to perform more efficiently. Another trend will be increased integration and changes in the design, allowing connectors to have multiple functions within a connector, such as hybrid solutions carrying different power and data transmissions. Lastly, customer-specific solutions will play an even more significant role in meeting the specific needs of different medical devices and patient populations.
Rick Lopez is a senior sales engineer and project manager at binder group subsidiary binder USA.
Paul Pulkowski is a marketing manager at binder USA and a specialist in circular connectors.
Jana Wagner is a product manager at binder, responsible for medical-grade connectors and other customer-specific projects.
How to submit a contribution to MDO
The opinions expressed in this blog post are the author’s only and do not necessarily reflect those of Medical Design & Outsourcing or its employees.