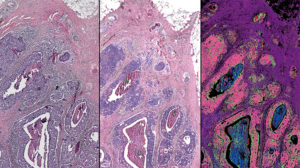
This comparison of a breast tissue biopsy shows a tissue sample dyed by traditional methods (left), a computed stain created from infrared-optical hybrid imaging (center) and tissue types identified with infrared data (right). The pink in this image signifies malignant cancer. (Image by Rohit Bhargava)
Researchers at the University of Illinois at Urbana-Champaign believe they may have brought cancer detection into the digital age, and at an affordable price.
The gold standard of tissue pathology is to add dyes or stains so that pathologists can see the shapes and patterns of the cells under a microscope. However, it can be difficult to distinguish cancer from healthy tissue or to pinpoint the boundaries of a tumor, and in many cases diagnosis is subjective.
Infrared microscopy can measure the molecular composition of tissue and provide quantitative measures that can distinguish cell types, but infrared microscopes are expensive and the samples require special preparation and handling, making them impractical for many clinical and research settings.
The Illinois researchers sought to glean more information about the underlying molecular changes that drive cancer than the traditional dye method could provide, and to make such technology affordable. They developed a hybrid microscope by adding an infrared laser and a specialized microscope lens, called an interference objective, to an optical camera. The infrared-optical hybrid measures both infrared data and a high-resolution optical image with a light microscope — the kind that’s ubiquitous in clinics and labs.
“We built the hybrid microscope from off-the-shelf components,” said Martin Schnell, a postdoctoral fellow in the research group and first author of the paper, in a news release. “This is important because it allows others to easily build their own microscope or upgrade an existing microscope,”
Combining the two techniques harnesses the strengths of both, the researchers said. The hybrid microscope has the high resolution, large field-of-view and accessibility of an optical microscope. Furthermore, infrared data can be analyzed computationally, without adding any dyes or stains that can damage tissues. Software can recreate different stains or even overlap them to create a more complete, all-digital picture of what’s in the tissue.
The researchers verified their microscope by imaging breast tissue samples, both healthy and cancerous, and comparing the results of the hybrid microscope’s computed “dyes” with those from the traditional staining technique. The digital biopsy closely correlated with the traditional one.
Furthermore, the researchers found that their infrared-optical hybrid outperformed state-of-the-art in infrared microscopes in several ways: It has 10 times larger coverage, greater consistency and four times higher resolution, allowing infrared imaging of larger samples, in less time, with unprecedented detail.
“Infrared-optical hybrid microscopy is widely compatible with conventional microscopy in biomedical applications,” Schnell said. “We combine the ease of use and universal availability of optical microscopy with the wide palette of infrared molecular contrast and machine learning. And by doing so, we hope to change how we routinely handle, image and understand microscopic tissue structure.”
The researchers plan to continue refining the computational tools used to analyze the hybrid images. They are working to optimize machine-learning programs that can measure multiple infrared wavelengths, creating images that readily distinguish between multiple cell types, and integrate that data with the detailed optical images to precisely map cancer within a sample. They also plan to explore further applications for hybrid microscope imaging, such as forensics, polymer science and other biomedical applications.
“It is very intriguing what this additional detail can offer in terms of pathology diagnoses,” said bioengineering professor Rohit Bhargava, director of the Cancer Center at Illinois and leader of the research group. “This could help speed up the wait for results, reduce costs of reagents and people to stain tissue, and provide an ‘all-digital’ solution for cancer pathology.”
The group published its results in the Proceedings of the National Academy of Sciences. The National Institutes of Health supported this work.




![A photo of the Medtronic GI Genius ColonPro polyp detection system flagging a potential sign of colon cancer during a colonoscopy. [Photo courtesy of Medtronic]](https://www.medicaldesignandoutsourcing.com/wp-content/uploads/2024/04/Medtronic-GI-Genius-doctors-268x170.jpg)