Sinead Miller, CEO and cofounder of PathEx [Image from Sinead Miller]
By John Minichillo
An elite cyclist turned medtech researcher, Sinead Miller may be in her greatest race yet — developing technology to treat sepsis, a major killer in U.S. healthcare settings.
An overwhelming immune response to infection, sepsis affects about 1 million Americans a year, killing up to nearly a third of them, according to NIH. To combat it, Miller initially focused on developing nanoparticles to magnetically extract bacteria from the blood while working as a graduate research assistant in recent years at Vanderbilt University.
But although the lab successfully bound bacteria to the nanoparticles and removed them from small blood samples, the process wasn’t scalable to human blood volumes, Miller told Medical Design & Outsourcing. Miller needed to find another solution.
“I developed a mathematical model to simulate the design, and through computational modeling, I found it wasn’t going to work. This eventually led to the idea of using inertial force to separate bacteria from healthy blood components,” said Miller, now the co-founder and CEO of a startup called Path Ex.
Inertial force is already used to separate blood components in apheresis machines. This concept, combined with her experience with nanoparticles, led to the idea behind the Path Ex blood filtration technology, she explained.
Bad crash with a good outcome
Miller knows what it’s like to overcome a major challenge. Miller, who grew up competing in bike races, went to Marian University in Indianapolis on a cycling scholarship and joined the U.S. National Team with a goal to compete in the Olympics. Her dream came to an end in 2010, when a severe crash in the Netherlands caused severe brain injury and numerous broken bones. She was out of school for a year while she recovered.
“[The experience] inspired me to want get into medicine, but I knew I didn’t want to be a physician. I wanted to be the person developing the technology, so I went into biomedical engineering,” she told MDO.
As a woman in a male-dominated field, Miller said she’s never felt that gender prejudice held her back.
“There are fewer women in the field, but I can’t say I’ve had any negative experiences because of that.” she said. “When we go to pitch, the investors are mostly male, but that has never been an issue for us. It’s been fair.”
Bacteria are bad but so are the endotoxins
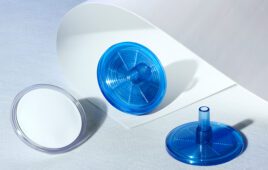
Technically not a filter, the Path Ex device works through adhesion. Using a dialysis-like device, it pumps blood through a helical channel that creates inertial forces to separate bacteria from healthy blood components, based on their size and shape. A coating in the channel binds to bacteria that are specific to pathogens and endotoxins. Referred to as a filter because it removes bacteria from the blood, treatment with the device takes about the same time as a hemodialysis session, anywhere from four to 24 hours.
Miller said that the applications for the Path Ex device could extend beyond sepsis, noting that a few small tweaks would allow it to target blood-borne diseases. And, she noted, it can do something that antibiotics can’t do: physically eliminate bacteria cells.
John Kellum, professor of critical care medicine at the University of Pittsburgh and director of the Center for Critical Care and Nephrology, said bacterial die-off often leads to a common side effect of antibiotic treatment.
“An example of that happens very commonly when patients are admitted who are ‘teetering on the brink.’ They’re given antibiotics and before they get better, they get worse,” Kellum explained. “Most of the antibiotics that we use, by virtue of killing the bacteria, actually release bacterial products into the bloodstream. Therefore, there could be a role in the use of something to clean up the blood of bacterial products even in the setting of effective antibiotic therapy.”
In the end, however, removing endotoxins could prove the more significant benefit of the Path Ex device. That’s because these by-products cause a massive reaction in about a third of sepsis patients, Kellum said.
“The reason endotoxin hurts you is not because it’s intrinsically toxic, but because it binds with a receptor and then causes a massive endogenous inflammatory reaction. About one-third of the patients with septic shock have detectable levels of endotoxin in the bloodstream, at least at some point. And the more they have the worse they do,” Kellum explained.