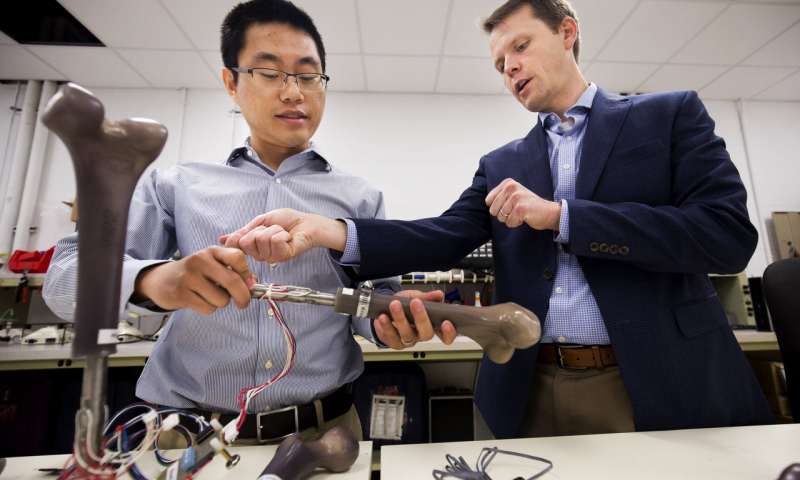
Dr. Jerome Lynch (right), an engineering professor at the University of Michigan, discusses the results of an experiment with research fellow Wentao Wang. The Office of Naval Research is sponsoring Lynch’s work on the Monitoring OsseoIntegrated Prostheses (MOIP)-a “smart” artificial leg equipped with specially designed sensors to monitor walking gait, alert users to prosthetic wear and tear, and warn of potential infection risk. (Credit: Joseph Xu/Senior Multimedia Content Producer, University of Michigan – College of Engineering)
Traditional leg prosthetics enable amputees to maintain mobility and lead more active lives. But these prosthetics depend on soft limb tissue to function and can be painful to wear, resulting in awkward walking motion and possible skin infection.
To improve the options available to warfighters, the Office of Naval Research (ONR) is partnering with Walter Reed National Military Medical Center, the Naval Research Laboratory and several universities to develop a “smart” artificial leg—equipped with specially designed sensors to monitor walking gait, alert users to prosthetic wear and tear, and warn of potential infection risk.
It’s called the Monitoring OsseoIntegrated Prostheses, or MOIP.
“This new class of intelligent prostheses could potentially have a profound impact on warfighters with limb loss,” said Dr. Liming Salvino, a program officer in ONR’s Warfighter Performance Department. “MOIP not only can improve quality of life, but also usher in the next generation of prosthetic limbs.”
Leg prosthetics most commonly fit amputees’ residual limbs via a socket that encloses the limb like a wooden clog. Because the socket exerts pressure on the limb’s soft tissue, pain and chafing, sores and blisters, and infection can occur. Amputees often must have their socket prosthetics adjusted regularly, which is inconvenient and costly. Consequently, many amputees give up prosthetics for wheelchairs.
MOIP uses an alternative limb type called an osseointegrated prosthetic—which includes a titanium fixture surgically implanted into the thigh bone, or femur. Bone grows, or “osseointegrates,” at the connection point with the implant, leaving only a small metallic connector protruding from the remaining leg. An accompanying artificial limb then can be attached or detached at will. The same procedure can be performed for upper limbs.
The advantages of osseointegrated prosthetics include less pain, a fluid walking motion and a more stable, better-fitting limb. But because metal sticks out of the residual limb, infection is a constant risk. To address this issue, MOIP will focus on infection detection, eradication and prevention—by developing both electrochemical sense-and-respond approaches and “smart” skin technologies.
This includes a critical bio-compatible sensor array embedded within an amputee’s residual limb—coupled with additional sensors on the osseointegrated prosthetic itself. The first technology of its kind, the array tracks changes in body temperature and pH balance, indicators of possible infection. It also monitors how well the bone and prosthetic limb fuse together and heal, allowing doctors to dramatically speed the recuperation process of warfighters.
Over time, the sensors evaluate the prosthetic’s strength, how much stress a user’s body places on it, and any changes to movement and walking gait.
“One game-changing application of this technology would be as a tool to inform doctors when prosthetics can be safely loaded after surgery, leading to more accurate determination of when patients are ready for physical therapy after receiving a new prosthetic,” said Dr. Jerome Lynch, a University of Michigan engineering professor who is overseeing the sensor array’s development. “Right now, doctors study X-ray images of a limb when making that determination.
“Because the sensors transmit information wirelessly, doctors also could potentially study patient data via a handheld reader,” said Lynch. “Think of it as an extremely specialized Fitbit. This could dramatically improve the recovery and long-term quality of life for patients.”
Lynch and his team successfully created a MOIP sensor array prototype using osseointegrated prosthetics and synthetic bone models manufactured onsite at the University of Michigan. While this prototype was successful in laboratory tests, they hope to have a new, improved model ready for clinical trials early next year.




