Sepsis happens to be a big deal. Hospital patients are often susceptible to sepsis, a bacterial infection that is the fifth leading cause of death. The standard of care is a blood culture followed by a round of antibiotics. There are about 25 million blood cultures performed each year in the United States.
Because of the high risks associated with sepsis, more than half of the blood samples are collected in an emergency setting. But the process of getting a blood sample using aseptic practices is 25 steps.
“And you’ve got to remember that the process is all happening when a patient may be running a fever, showing a rapid respiratory rate, or hypotensive crisis,” noted Greg Bullington, co-founder and CEO of Magnolia Medical. “There is real concern that the patient has a bloodstream infection and speed to diagnosis is critical.”
If a blood culture indicates a positive result, a clinician from the lab will phone down to the physician on the floor and notify them of the early result. Because of the health risk and time factor, that initial analysis is usually enough to make a practitioner prescribe antibiotics.
However, in some cases, that positive result could be the result of a contaminant. The false positive rate is about 3-4%, which represents one-third to one-half of positive blood cultures. Many of those patients might see a negative response to the antibiotic regimen (e.g., an allergy or development of C. Diff).
The decision on the part of the practitioner is understandable, but the result of a false positive is a waste of hospital resources and an unnecessary tax on a person’s microbiome.
A decade ago, Bullington founded Magnolia with Dr. Richard Patton, a retired pathologist and medical director.
During his tenure as a practicing physician, Patton was able to observe the downstream consequences of inappropriate antibiotic use. He became convinced that the mortality caused by allergic reactions or onset of C. Diff infections could be alleviated through better application of antibiotics. “Patton was convinced that this was a problem worth solving,” said Bullington.
Bullington put it this way: “We realized we could create a ton of value for patients by getting rid of these false positives, and eliminating the noise so that every time we have a positive, we know we actually have a septic patient.”
Finding the right path
 Magnolia used its knowledge to create SteriPath, a closed-loop blood collection system that eliminated the risk of contamination. “We determined that an automated mechanical device eliminated the chance for human error,” Bullington explained.
Magnolia used its knowledge to create SteriPath, a closed-loop blood collection system that eliminated the risk of contamination. “We determined that an automated mechanical device eliminated the chance for human error,” Bullington explained.
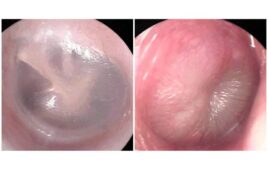
SteriPath is a self-contained, pre-assembled, sterile blood collection system. It provides proprietary vein-to-bottle technology that significantly reduces blood culture contamination.
Blood is drawn by a healthcare practitioner from the patient (typically from a vein in the arm). The SteriPath system diverts the initial portion (1.5 to 2.0 milliliters) of the blood draw into a separate chamber, safely sequestering skin and other contaminants. A new, second sterile blood flow path is then created allowing the remainder of the blood sample to be collected in the culture bottle and sent to the lab.
“With our product, we can get physicians out of the undesirable, unenviable position of getting bad information and using it to make bad treatment decisions,” Bullington said.
Magnolia has shown through research that its product can reduce false positives. A recent study at the University of Nebraska Medical Center (UNMC) found that the device leads to an 88% reduction in false positives.
Fitting into a value conversation
Bullington said Magnolia fits neatly into the policies associated with value-based medicine. “Some of the key tenets of transparency, accountability, and continual performance improvement—these are all really good things for medicine.”
Magnolia has been able to connect with hospitals that have a reported standardized infection ratio (SIR) that exceeds thresholds and puts them over the penalty market from a CMS perspective. “Those rates are partially attributable to the false positive diagnostic test results like blood cultures,” he said.
It is a significant value for the hospitals to get rid of erroneous test results that end up having a negative impact on both on those reporting rates and on multi-drug resistant organism infection rates.
Further, hospitals are motivated under bundled payment systems to eliminate complications and downstream resource consumption that might be avoided. “It saves the hospital a significant amount of money if they can virtually eliminate false-positive blood cultures,” Bullington said. “They don’t have to do extra microbiology and hematology testing, and they don’t administer inappropriate antibiotics.”
Even better, said Bullington, they don’t put a patient at risk of contracting an HAI, pneumonia or C. Diff, because of a longer hospital stay. Hospitals don’t get reimbursed for such maladies, but are burdened with all the costs of treating that patient.
Breaking hospital inertia
“When you can bring all that to the table, so you are effectively delivering an outcome with no risk to the institution, but still not getting a jump from hospitals—that’s where the logic breaks, said Bullington.
“At that point, you kind of scratch your head and ask, ‘Why haven’t we been able to turn the system on its head overnight?’”
Today, SteriPath is considered a successful product. But Bullington said it took a lot of sweat to get here. “It can be so difficult to break inertia in a hospital.”
He described a typical meeting in which he’ll come in and show 10-fold better performance over the current practices. “That’s a game changer. People tell us they’ve been trying to solve the problem for a long time.”
Bullington noted that getting hospitals to believe in the product isn’t the issue. It’s getting them to act. The biggest challenge at hospitals is prioritization.
“If you talk to any chief medical officer or CFO, they will list 100 things they could do tomorrow to move the needle on quality, save money, and be good for patients and the hospital—so how do you prioritize which ones to pursue?”
This question, said Bullington, is the tenet on which a medical product will succeed or fail.
Magnolia has been able to leverage the recent Joint Commission and federal mandates on antibiotic stewardship that hospitals must follow. Bullington said the mandate has provided a tailwind to move Magnolia to the tops of many hospital’s priority lists.
In the future Magnolia also plans to introduce multiple platforms and products to address testing inaccuracies. Bullington said the ultimate goal is to change the standard of care. “Our top-level goal is to eliminate the variability in in-vitro diagnostic testing. If we can do that, we can put physicians in a position where they have the best information possible so they can make the best decisions and deliver the best outcomes.”
That, he says, is what value-based care should be—getting the right information at the right time to the right people to make the right decisions.
[Want to stay more on top of MDO content? Subscribe to our weekly e-newsletter.]