CLEVELAND, April 5, 2013 /PRNewswire/ — The first-in-human study of the NeuroBlate™ Thermal Therapy System finds that it appears to provide a new, safe and minimally invasive procedure for treating recurrent glioblastoma (GBM), a malignant type of brain tumor. The study, which appears April 5 in the Journal of Neurosurgery online, was written by lead author Andrew Sloan , MD, director of Brain Tumor and Neuro-Oncology Center at University Hospitals (UH) Case Medical Center and Case Comprehensive Cancer Center, who also served as co-Principal Investigator, as well as Principal Investigator Gene Barnett , MD, director of the Brain Tumor and Neuro-Oncology Center at Cleveland Clinic and Case Comprehensive Cancer Center, and colleagues from UH, Cleveland Clinic, Cleveland Clinic Florida, University of Manitoba and Case Western Reserve University.
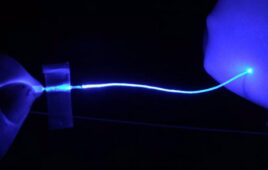
NeuroBlate™ is a device that “cooks” brain tumors in a controlled fashion to destroy them. It uses a minimally invasive, MRI-guided laser system to coagulate, or heat and kill, brain tumors. The procedure is conducted in an MRI machine, enabling surgeons to plan, steer and see in real-time the device, the heat map of the area treated by the laser and the tumor tissue that has been coagulated.
“This technology is unique in that it allows the surgeon not only to precisely control where the treatment is delivered, but the ability to visualize the actual effect on the tissue as it is happening,” said Dr. Sloan. “This enables the surgeon to adjust the treatment continuously as it is delivered, which increases precision in treating the cancer and avoiding surrounding healthy brain tissue.”
The study was a Phase I clinical trial investigating the safety and performance of NeuroBlate™ (formerly known as AutoLITT™), a specially-designed laser probe system. The FDA gave the system’s developer Monteris Medical and the Case Comprehensive Cancer Center, (comprised of the UH Case Medical Center, Cleveland Clinic , and Case Western Reserve University School of Medicine), an investigatory device exemption (IDE) to study the system in patients with GBMs. The device has recently been cleared by the FDA due, in part, to the results of the study.
The paper describes the treatment of the first 10 patients with this technology. These patients, who had a median age of 55, had tumors which were diagnosed to be inoperable or “high risk” for open surgical resection because of their location close to vital areas in the brain, or difficult to access with conventional surgery.
“Overall the NeuroBlate™ procedure was well-tolerated,” said Dr. Sloan. “All 10 patients were alert and responsive within one to two hours post-operatively and nine out of the 10 patients were ambulatory within hours. Response and survival was also nearly 10 ½ months, better than expected for patients with such advanced disease.”
“Previous attempts using less invasive approaches such as brachytherapy and stereotactic radiosurgery have proven ineffective in recent meta-analysis and randomized trials,” said Dr. Barnett. “However, unlike therapies using ionizing radiation, NeuroBlate™ therapy results in tumor death at the time of the procedure. A larger national study will be developed, as a result of this initial success.”
Dr. Sloan and Dr. Barnett are paid consultants for Monteris Medical and members of the company’s Medical Advisory Board.