For years, telemedicine has been regarded as a care delivery model for the future with extensive barriers to overcome. While many of these barriers—most importantly policy and reimbursement—persist, research and provider experience has proven that telehealth delivers better patient care, more effectively and less expensively. Today, while politicians debate expanding Medicare’s coverage of telehealth, providers focused on improving patient care are implementing telehealth delivery models.
World’s first virtual care center
Last fall in Chesterfield, Mo., Mercy health system opened a “bedless” hospital that relies completely on telehealth to deliver care. Called Mercy Virtual Care Center, this telemedicine facility’s large medical team provides Mercy’s 46 hospitals with access to stroke specialists, remote ICU monito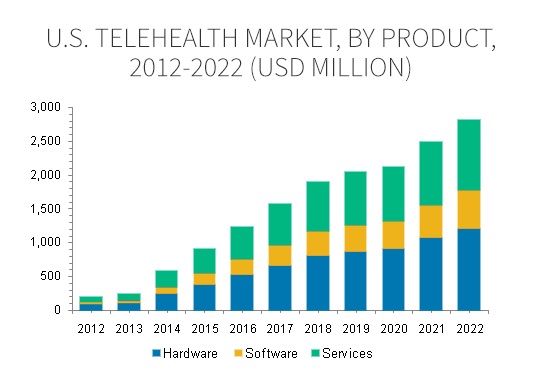 ring and other telehealth services. The center is equipped with two-way cameras, online-enabled instruments and real-time vital signs that allow providers to “see” patients in a traditional hospital, a physician office and the patient’s home.
ring and other telehealth services. The center is equipped with two-way cameras, online-enabled instruments and real-time vital signs that allow providers to “see” patients in a traditional hospital, a physician office and the patient’s home.
Saving lives with telestroke
The programs at Mercy bring together in one place uses of telehealth already implemented at hospitals and health systems throughout the country. Telestroke, for example, has been in use for 20 years and a search on telestroke in Google Scholar returns almost 66 references to research and studies published in 2015 and 2016 alone. In 2012, there were 56 telestroke programs in the country each serving an average of 7 hospitals. One provider of telestroke technology, InTouch Health, says its services touch 60,000 patients annually and supports a stroke consult every 9 minutes.
The impact of telestroke on patient lives is significant. By speeding delivery of both clot busting drugs and providing fast diagnosis so that patients and be quickly transferred to centers to receive endovascular treatments (a process for removing blood clots in the brain), telestroke both saves lives and can virtually eliminate the long-term impact of stroke. As one stroke neurologist working at a telestroke center put it, “I see miraculous recoveries on a weekly basis.”
Mobile devices bring specialist to patient bedsides
With the addition of mobile devices (including iPads, laptops and Smartphones), telehealth can move quickly and easily to bedsides allowing doctors to access specialists quickly and easily. A 2015 study shows that pediatric evaluations of children in an ER through FaceTime connections using an iPad were as effective as bedside evaluations. For small, rural hospitals, access to specialists using this type of connection brings big-city care to small town patients.
A growth market for better outcomes
In light of the positive outcomes from telehealth, it’s no surprise that market research firms are predicting significant market growth. An October 2015 report from Grand View Research sizes the telehealth market at $2.8B by 2022 with the bulk of that growth coming the increased use of telehealth by hospitals and health systems. On the savings side, research firm Avalare Health reported in January that changes to Medicare policy regarding coverage of telehealth and remote patient monitoring could save $1.8M.
Reprinted with permission.




