Theradaptive founder and CEO Luis Alvarez discusses how his team’s groundbreaking novel protein engineering platform promises to unlock the vast potential of therapeutic proteins in regenerative medicine, trauma and oncology.
By Luis Alvarez, Theradaptive

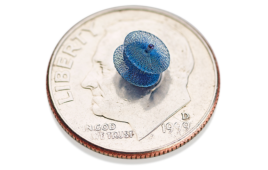
Theradaptive’s OsteoAdapt SP is a resorbable spinal fusion implant with a bioactive surface coating. [Photo courtesy of Theradaptive]
Harnessing the power of proteins is not a new concept. The first Nobel Prize in Physiology or Medicine was awarded in recognition of the discovery and use of a therapeutic protein, an antibody-based treatment for diphtheria. More than 100 years later, the therapeutic applications of proteins are vast and span almost every branch of modern medicine.
But we have yet to harness much of the vast potential of therapeutic proteins to repair and regenerate tissue, partly because we lack the ability to reliably target the activity of a protein to a specific location in the body with anatomical precision for an extended period of time. Currently, the naturally occurring proteins used to regenerate bone disperse away from the site where they are needed, leading to off-target effects such as bone growth and inflammation elsewhere in the body.
This is the problem Theradaptive is on a mission to solve. Our unique protein engineering platform enables us to modify bioactive proteins to create variants that bind to implants or devices and can be applied to the surface of an implant like a coat of paint. This enables the precision delivery and control of that protein through placement of the implant, optimizing efficacy where it is needed and removing the risk of off-target effects and toxicity.
Benefits beyond binding
Proteins initiate cell signaling that drives tissue repair and regeneration, but there needs to be an elevated presence of that protein for a sustained period generally ranging from days to months. There have been technologies that use encapsulation techniques or timed-release mechanisms to maintain sufficient protein levels at the site of repair, but a downside to these is that the majority of therapeutic protein is sequestered and not available to the damaged tissues at any given time, limiting efficacy.
Our approach overcomes this by coating the device or implant with a stable layer of the therapeutic protein, which ensures that the entire therapeutic dose is available all of the time to interact with cells and initiate the required repair-signaling pathways. By making the entire surface of the device or implant bioactive, we maximize the surface area that can interact with cells, maximizing the efficacy of the protein.
Navigating protein complexity

Theradaptive’s OsteoAdapt SP wet in a cage [Photo courtesy of Theradaptive]
We have developed novel computational methods that streamline this process and allow us to mine large sequence libraries to identify variants of existing therapeutic proteins that have promising binding potential.
We then take those promising variants and repeatedly modify and refine them using our own bioinformatics resource to focus that refinement toward the additional characteristics we want — stronger binding or enhanced stability, for example — without impacting therapeutic activity. It’s a computationally informed, accelerated evolution that results in a protein variant that is primed for highly desirable combined efficacy, stability and substrate binding. This refinement is possible for many proteins of therapeutic interest because the region of the molecule that is therapeutically active constitutes a very small part of the overall molecule.
Compared to the complexity involved in producing an optimized material-binding variant of a therapeutic protein, the application of that protein to the chosen carrier — such as an implant or another device — is relatively simple: the carrier can be simply dipped in a liquid formulation of the protein for a few minutes. When properly optimized, the protein variant behaves like a paint that coats the surface of the implant or device, creating a stable surface layer of bioactive protein.
Stabilizing proteins as a surface layer in this way also has other advantages, as it renders them far more robust and stable than free proteins in solution. In an unexpected application of this phenomenon, we have developed methods that permit us to terminally sterilize implants and devices coated with bioactive proteins without impacting the clinical efficacy of the bound protein. This results in manufacturing workflows that do not require aseptic techniques, vastly simplifying the process and reducing costs. The resulting product also shows excellent thermal stability, allowing terminally sterilized products to be stored at room temperature.
Reducing development risk and accelerating the regulatory path

Theradaptive’s OsteoAdapt SP can be combined with blood or marrow before placement in a patient. [Photo courtesy of Theradaptive]
For example, bone morphogenetic protein 2 (BMP2) drives bone formation and has been used in various orthopedic indications for over 20 years. But without a way to deliver it with anatomical precision and prevent it from dispersing to other areas of the body, its use has been associated with significant off-target effects including heterotopic bone formation and severe edema.
To address this, we used our protein engineering platform to create a material-binding, or “sticky,” variant of BMP2 that we call AMP2. AMP2 retains the naturally occurring osteoinductive properties of BMP2, but delivers bone growth in a targeted anatomically precise manner. Our lead product, OsteoAdapt SP, is a resorbable spinal fusion implant with a bioactive surface coating of AMP2. This enables the precision placement of this powerful bone formation protein in the exact location where it is needed to maximize therapeutic effect while eliminating off-target effects associated with BMP2.
OsteoAdapt SP has been granted three FDA Breakthrough Device Designations due to its clinical potential and the promise of improvement over current therapeutics. These designations permit the acceleration of regulatory review and clinical development to deliver this much-needed innovation in spinal fusion to patients.
Fertile ground to drive our transformation
With our first clinical trial for OsteoAdapt SP beginning in late March, it is a pivotal moment for Theradaptive. We are now a clinical-stage company, and embarked on this transformation from the strongest of foundations.
When Theradaptive was formed, we chose to locate in Frederick, Maryland to be part of the world-leading life sciences ecosystem that Maryland has to offer. The wealth of support from local and state agencies such as the Maryland Stem Cell Research Fund (MSCRF) and technology incubators such as the Frederick Innovative Technology Center (FITCI)were instrumental to our early progress. We are now at an entirely different stage as a company, but the resources, infrastructure and talent we can tap into given our location will continue to put us in the best position to accelerate growth and allow us to expand our world-class team for the journey ahead.
In 2024, we look forward to collecting our first clinical data, as well as continuing to develop our pipeline of targeted protein therapeutics for indications beyond orthopedics and spine. In 2023, we launched a program in tumor targeted immuno-oncology, thus extending our platform in a promising new direction.
Ultimately, we seek to harness the hidden power of proteins to not only exert their expected therapeutic effect, but to also allow us control their fate once placed inside the body.

Theradaptive founder and CEO Luis Alvarez [Photo courtesy of Theradaptive]
How to submit a contribution to MDO
The opinions expressed in this blog post are the author’s only and do not necessarily reflect those of Medical Design & Outsourcing or its employees.