Age-related macular degeneration, a disease that slowly degrades light-sensitive cells in the retina, is the leading cause of vision loss and blindness among people 65 and older, according to the Centers for Disease Control and Prevention. Doctors can’t prevent such loss of sight – but a system that replaces light-sensitive cells designed by Daniel Palanker, a professor of ophthalmology, may ease the burden.
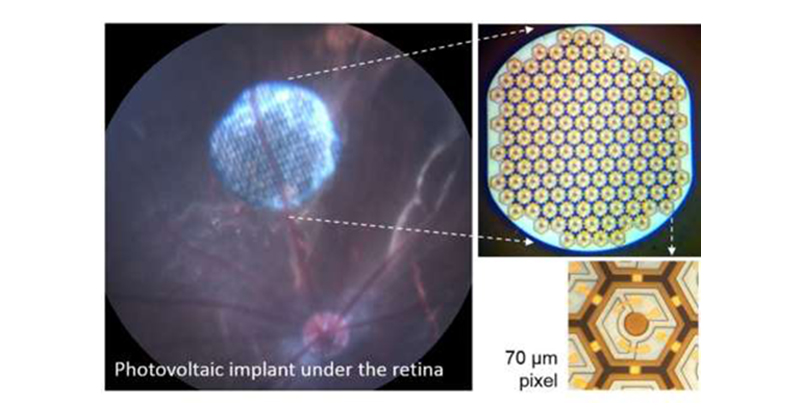
The device – a combination of image-processing goggles and tiny silicon chips implanted in the retina – has been more than a decade in the making. Although the device’s resolution is not yet where its designers hope to get it – currently the technology can only reach 20/200 vision, which is not enough to read clearly or drive safely – a five-patient feasibility study has begun in Paris, with a second planned later in the year in the Eastern United States.
the Eastern United States.
“We published the first concept paper of how we would approach this 12 years ago, and now we’ve validated in human patients basically all the key assumptions we made on the way,” said Palanker, who is also the director of the Hansen Experimental Physics Laboratory and a member of Stanford Bio-X and the Stanford Neurosciences Institute.
Too many wires
Palanker had been interested in how eyes function since his graduate studies in applied physics. Until the early 2000s, most of Palanker’s research focused on the use of lasers in eye surgery.
Then he learned about artificial retinas, assistive devices intended to treat patients who have lost some of the light-sensitive cells in their retinas to diseases such as age-related macular degeneration or retinitis pigmentosa.
But artificial retinas that were then in development had a number of drawbacks. For one thing, none of them achieved decent resolution. At the time, the best artificial retina corresponded to about 20/1200 vision.
In addition, most devices in the early 2000s needed many wires. Some systems implanted a camera directly into the eye, which required elaborate wiring just to power it. Other devices mounted the camera onto glasses and fed the images through a cable to an electrode array placed on the retina. All the options demanded invasive, complex surgery and long-term maintenance issues, including managing problematic cables that crossed the eye wall, sometimes affecting the remaining healthy rods and cones.
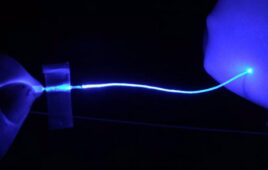
The wireless retinal implants convert light transmitted from special glasses into electrical current, which stimulates the retina’s bipolar cells. Credit: Palanker lab
Delivering light
Palanker thought he could do better using a purely optical approach. As he imagined it, patients would wear special goggles that would convert ambient light into normally invisible infrared images and project those images into the eye in a manner similar to augmented-reality glasses. Photovoltaic cells – essentially tiny solar panels – implanted under the damaged parts of the retina would pick up the infrared images and convert them into electrical signals, replacing the function of damaged rods and cones.
“I thought that the eye is a beautiful optical system, where information and power can be delivered by light, and this would eliminate the need for wires and make surgery much less invasive,” Palanker said. In addition, it would be easier to miniaturize the photovoltaic sensors, thus improving resolution. Palanker’s device provides an added benefit as well: because the implanted sensors would only replace damaged rods and cones, patients could still see normally with the parts of their retinas that hadn’t been damaged.
By 2005, Palanker and colleagues had published a plan for how their device would work, and in 2008 they won a Bio-X seed grant to begin building a device and testing this idea in rodents.
The next phase
Pixium Vision, the company that licensed the photovoltaic retinal prosthesis, or PRIMA, technology in 2013, manufactured a device for humans and got approval for clinical testing in late 2017. Clinical trials started last month, and so far three patients have been implanted with the device. Those surgeries went well, Palanker said, and patients report seeing bright white patterns in their formerly damaged areas, within the resolution limits researchers had expected. Thorough testing is now being conducted to assess the quality of this prosthetic vision, including how well patients can make out various shapes and letters.
The researchers still face important challenges – most importantl, further improving resolution. Right now, pixels in human implants are 100 micrometers in size, and tests demonstrated that 50 micrometer pixels also work well, providing spatial resolution equivalent to about 20/200 vision. Eventually, Palanker would like to get it to 20/40 – what the state requires for a driver’s license – and the lab expects to publish a new design for achieving that resolution later this year, he said. The researchers are also developing better ways of processing images, so that patients can distinguish objects more easily.
“We are addressing one of the largest unmet needs in incurable blinding conditions,” Palanker said. “It’s very exciting.”
Feature Photo Credit: Professor Daniel Palanker works with CS senior Jack Boffa on software for simulation of prosthetic vision and for augmented reality goggles which activate the retinal implant. (Image credit: L.A. Cicero)