[Image from New York Genome Center]
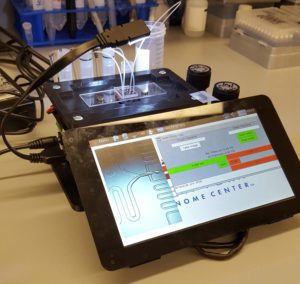
Single-cell analysis is a way for researchers to study how cells influence disease and their response to treatment, but there is a lack of cost-effective and user-friendly devices to help. Researchers at the New York Genome Center and New York University have attempted to alleviate those barriers and enable broader access to single-cell analysis by creating a 3D-printed, portable, low-cost microfluidic controller.
The researchers used the device to study synovial tissue from patients who have rheumatoid arthritis at the Hospital for Special Surgery. The study showed that using a 3D-printed custom device with electronic and pneumatic components was easy to get and only cost about $600 to assemble.
“Most commercial microfluidic instruments are very costly; as a result, not every lab has access to exciting technology for single-cell analysis,” William Stephenson, senior research engineer and lead author on the study, said in a press release. “We designed the instrument to perform droplet microfluidics and in particular Drop-seq, a massively parallel technology for single cell RNA-sequencing.”
The researchers used the device to analyze joint synovial tissue from rheumatoid arthritis patients. Since the controller is portable, the researchers could then process the samples on-site immediately following surgery.
They collected samples from five rheumatoid arthritis patients and had 20,387 cells to analyze and find gene expression patterns for each cell.
“This dataset gave us the opportunity to identify individual sub-populations of cells that could drive the progression of rheumatoid arthritis, even if they have not been previously characterized,” Rahul Satija, senior author on the study, said.
Analyzing the complete dataset and looking for groups of similar cells allowed the researchers to identify 13 groups that represented infiltrating immune and inflamed stromal populations. The researchers were interested in the distinct groups of fibroblasts that had very different gene expression patterns.
“Roughly an hour after surgical excision, individual cells from patient tissues were labeled for single-cell sequencing. From this work, we have classified unrecognized fibroblast subtypes that may prove to be important drug targets for our rheumatoid arthritis patients,” said Laura Donlin, lead author on the study.
Using flow cytometry, the researchers could confirm the presence of multiple groups of fibroblasts and discovered that they had distinct localization patterns with joint tissue.
The researchers hope that the new dataset created by the device can create a comprehensive “cell atlas” for synovial tissue for rheumatoid arthritis patients. They also hope to get samples from other sthritic conditions like psoriatic and osteoarthritis. The researchers also plan to use CITE-seq to more accurately classify cell types by measuring the presence of surface proteins as well as the transcriptome.
“We hope that this instrument lowers the hurdles associated with performing single-cell transcriptome profiling experiments in basic research and clinic settings,” Stephenson said.
The research was published in the journal Nature Communications.




