The U.S. economy, national security, and a war on opioids? One of the latest issues popping up during this 2016 election cycle focuses on opioid addiction and abuse. President Obama, candidates from both sides, the Center for Disease Control (CDC), even medical schools are all urging doctors to cut back on opioid prescriptions. Just days ago, the president suggested that fighting opioid abuse is as important as fighting terrorism. His administration recently released details of its $1.1 billion proposal to curb drug abuse.
According to the CDC, every 19 minutes an American dies from an opioid overdose (a statistic that includes heroin as well as prescription drugs), making it the leading cause of unintentional deaths in the U.S. This figure prompted the CDC to release new suggested guidelines for physicians that prescribe opioids for chronic pain. Kicking off the CDC’s 12 recommendations is a passage plainly stating that non-opioid therapies are preferred for chronic pain. The CDC added that, “Clinicians should consider opioid therapy only if expected benefits for both pain and function are anticipated to outweigh risks to the patient.”
The battle lines against opioids have been drawn, but are these messages resonating with physicians? According to Guidepoint’s Post-Surgical Pain Management TRACKER, there’s been a small decline in the opioid treatment share for major joint replacements, but opioids continue to be the preferred therapy.
Guidepoint’s Post-Surgical Pain Management TRACKER launched roughly one year ago to help subscribers track an increasingly debated therapy landscape. This TRACKER captures and delivers data on market share, adoption rates, treatment volumes, and other data points for the three major modalities used when treating moderate-to-severe post-operative pain: opioids, local anesthetics, and nerve blocks. Data is directly collected from clinical sites and physicians, not end-users.
Treatment Shares
With more than 12 months of treatment data collected, Guidepoint’s Post-Surgical Pain Management TRACKER shows a slow and steady trend of physicians exploring and moving to newer non-opioid therapies, such as Exparel and pumps. From January through December 2015, Exparel’s local injection treatment share grew 2.59 percent, while Exparel’s peripheral block share grew 0.68 percent. Ionsys, a newly approved, patient-controlled analgesia (PCA), also experienced an early uptake, increasing 1 percent in share. Ionsys, which was approved by the FDA last spring for in-hospital use, is a “needle free,” pre-programmed system that delivers fentanyl through a slight electrical current.
As these newer products grabbed more share, opioids and non-Exparel peripheral blocks saw reduced usage: oral opioids declined 1 percent while PCA opioids declined 2.84 percent. Treatment share for spinal/epidural nerve blocks and other peripheral blocks fell 1.5 percent and 2.21 percent, respectively. Treatment share for the third tracked modality, local anesthetics, grew 1.55 percent.
Tracking Length of Use
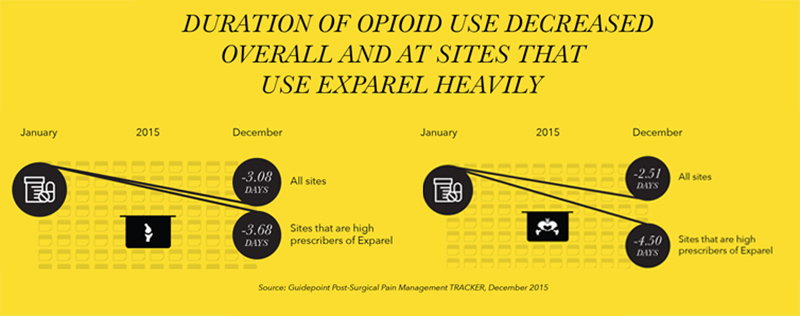
Guidepoint’s Post-Surgical Pain Management TRACKER found more pronounced variances when tracking how long patients use opioids, post-discharge, after knee and hip replacement surgeries. In 2015, there was an observed decline in the duration of post-surgical opioid use in knee and hip arthroplasty procedures. On average across all sites, duration of opioid use decreased by 3.08 days for knee replacement patients and 2.51 days for hip replacement patients over the course of 2015.
This trend was even more prominent at sites that report using Exparel in 75 percent or more of their arthroplasty procedures. These sites saw a decrease of 3.68 days for knee replacement patients and 4.5 days for hip replacement patients.
Looking to the future
Although 2015 saw a slight decline in opioid treatment share, TRACKER data finds that opioids are still used by the majority (90-95 percent) of post-operative arthroplasty patients. However, more than 30 percent of surveyed physicians expect an increase in the use of peripheral nerve blocks, such as adductor canal blocks, as an alternative to heavy opioids.
Many believe there is an evident need for alternative, non-opioid pain-management methods, but price and availability of studies are the biggest hurdles to widespread implementation.
“Hospitals are hesitant to pay for new and expensive products without proof of significant incremental benefit,” says Kenneth Wahl, Vice President of Guidepoint TRACKER. “Plus, physicians need to become more familiar with uses. Opioids are extremely effective, and generic formulations are just pennies per pill. Unfortunately some people don’t want to stop taking them after the pain stops.”
The entire Guidepoint TRACKER suite of data products monitors usage trends in the medical device and therapeutics markets, including cosmetic, spine, and bariatric procedures in the U.S.




