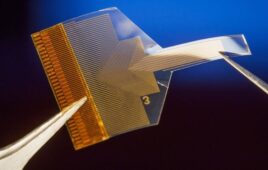
The electrodes are equipped with 128 sensors that can record extremely localized brain signals and 16 stimulation contacts that can deliver clinical grade stimulation currents and that can additionally record brain signals. [Image courtesy of UCSD]
Such technology could bring wireless monitoring of patients with treatment-resistant epilepsy for extended periods of time (up to 30 days) as they go about their daily lives.
Researchers also see broader applications, potentially helping those with Parkinson’s disease, movement disorders, obsessive-compulsive disorder, obesity, treatment-resistant depression, high-impact chronic pain and other disorders.
These sensors can record activity from large populations of individual neurons, with a resolution of as few as one or two neurons. A study recently published in Nature Communications demonstrated this ability in humans and a range of animal models. The research team is led by the Integrated Electronics and Biointerfaces Laboratory (IEBL) at UCSD.
The team calls the system the UCSD Micro-stereo-electro-encephalography (µSEEG). They can manufacture the technology at high volume and low cost because it’s derived from existing technologies used to manufacture digital display screens. Additionally, the manufacturing process enables a series of unique features for the depth electrodes.
This approach relies on ultra-thin, flexible and customizable probes made of clinical-grade materials with sensors that can record extremely localized brain signals. With probes smaller than today’s clinical sensors, they can be placed very close to one another. This allows for high-resolution sensing in specific areas at unprecedented depths within the brain.
According to the researchers, the probes can record with up to 128 channels, compared to only eight to 16 in clinical probes. The team believes they can expand the number of channels to thousands per probe with their unique manufacturing approach. This would enhance the ability to acquire, analyze and understand brain signals at a higher resolution. The researchers have also used the thin-film approach to create brain-computer interfaces (BCIs) that record activity and deliver therapeutic electrical stimulation to the surface of the brain cortex.
Developing the sensors
The researchers say their probes are monolithic, meaning their individual components are layered on top of one another to create a single, cohesive unit. They don’t require manual assembly of additional wires to conduct recordings. T
According to the researchers, their recording system is both customizable and scalable to manufacture thanks to the thin-film technology. The probes are about 1/5 the thickness of a human hair.
The team performed the design, manufacture, experimental testing and analysis of results from this system through a cross-disciplinary team of engineers, surgeons and medical researchers from UCSD, Harvard Medical School and Massachusetts General Hospital and Oregon Health and Science University.
“We developed an entirely different manufacturing method for thin-film electrodes that can reach deep brain structures – at a depth that is necessary for therapeutic reasons — enabling reproducible, customizable, and high-throughput production of electrodes but with a high spatial resolution and channel count despite a thinner electrode body. Additionally, the electrode insertion is compatible with existing surgical techniques in the operating room, lowering the barrier for their adoption in clinical procedures,” UC San Diego electrical engineering professor Shadi Dayeh, the corresponding author on the team’s research paper, said in a post on the university’s website.
Advancing the system
The researchers say their system is needed to identify the specific regions of the brain triggering seizures caused by treatment-resistant epilepsy. They want to develop a brain monitoring system with sensors both inserted deep within the brain and sensors on the surface of the brain.
Those sensors will communicate wirelessly with a small computer system in a wireless cap, which a person can wear for extended periods of time. The cap provides wireless power and the computational infrastructure to capture brain signals recorded for 30 days.
“We are currently focused on applying the technology to patients with treatment-resistant epilepsy. The ultimate goal is to advance the system and related required technologies by 2026 to give patients access to a wireless system that allows them to move freely within the hospital environment and then at home, without being tethered to any machinery, while cortical and deep brain structures are monitored continuously for up to 30 days,” Dayeh said.
In the paper, the team used the system in two human patients. They also offered data from a series of different animal models.