For patients affected by lung diseases such as pulmonary fibrosis, chronic obstructive pulmonary disease, cystic fibrosis, and others, cures for their diseases are incredibly rare, if not nonexistent.
“We really have no option, but to offer them a lung transplantation,” says Vibha Lama, MD, a professor of internal medicine and associate chief of basic and translational research at Michigan Medicine’s Division of Pulmonary and Critical Care Medicine.
“Survival of lung transplantation is worse than all other solid organ transplants,” she says. “The five-year survival rate is only 50 percent, and the 10-year survival rate is as low as 20 percent. For me to tell my patient that this second chance at life comes with this critical limitation is incredibly hard.”
Lama explains that in many lung transplant patients, the body will chronically reject the new lung.
“Small airways of the transplanted lung, or graft, begin scarring and slowly become completely scarred and close up. This process is called bronchiolitis obliterans syndrome (BOS),” she says. “The patient will begin to have shortness of breath again, like they did before the transplant, and this scarring can lead to graft problems and ultimately death in some patients. Right now we have nothing to prevent or stop this scarring process once it begins.”
Lama is the senior author on a new paper, published in the Journal of Clinical Investigation, which examined the scarring process in transplanted lungs in hopes of identifying novel therapies to stop scarring before it starts.
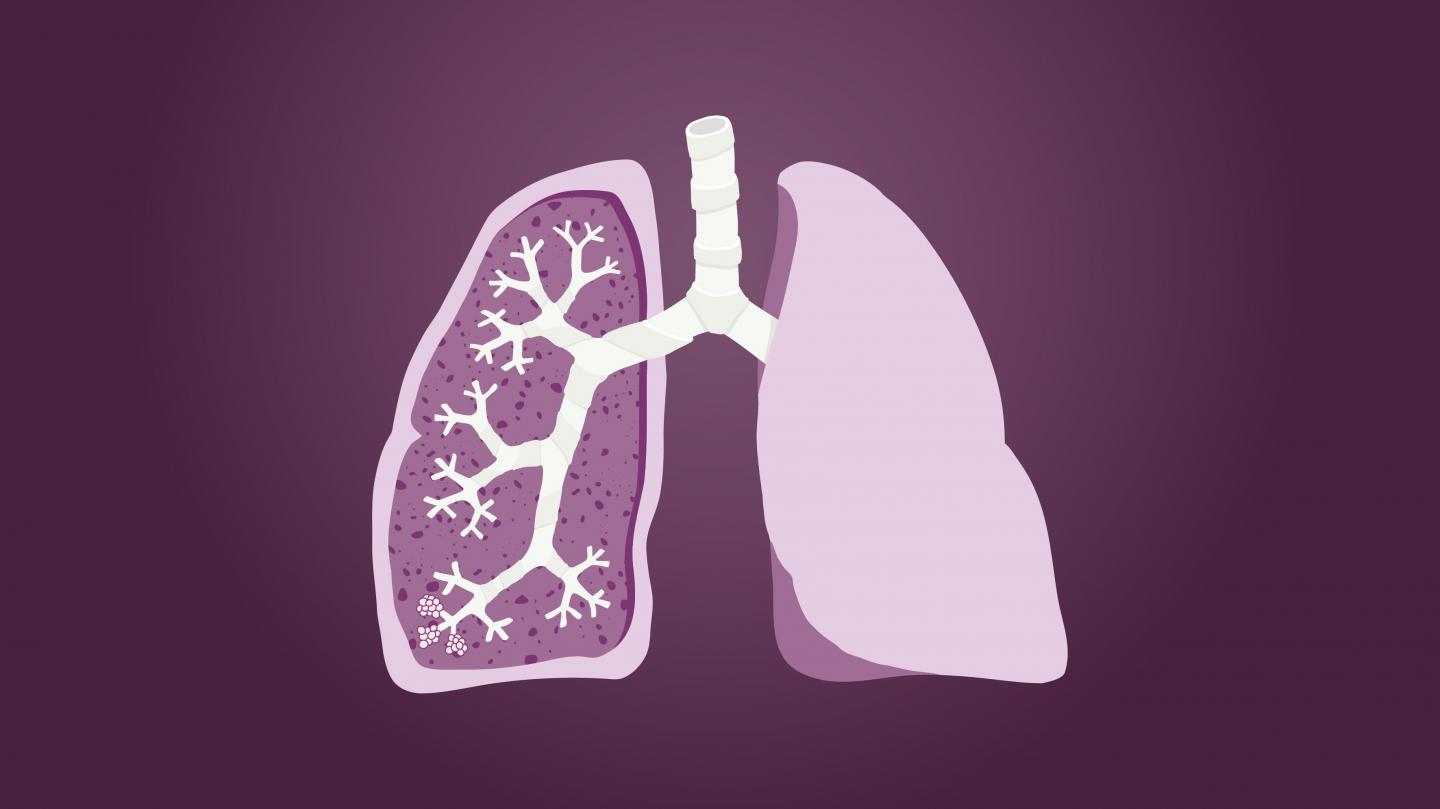
(Image credit: Michigan Medicine)
“This study is unique because it actually started from our patients,” Lama says. “Samples were collected from lung transplant patients by going into the lung with a small scope that helps us to insert a liquid into the lung and draw it back, allowing us to study the internal environment of the transplanted organ. This procedure, called bronchoalveolar lavage, is routinely done to rule out acute rejection or infection.”
In 2007, in a study published in JCI, Lama’s team demonstrated that they could isolate novel mesenchymal stem cells from this bronchoalveolar lavage.
In this new study, Lama and team focused on cells harvested from lung transplant patients who had BOS and those who did not.
“We started investigating cells in patients who have BOS and found that even after being removed from the fibrotic graft, these cells stayed activated, making more collagen, which explained their ability to promote relentless scarring,” Lama says.
As the team dug into what keeps these cells activated, they discovered a chain of upstream signals starting with autotaxin, an enzyme which acts on the cell membrane to generate lysophosphatidic acid. This potent lipid mediator was signaling the cells to produce more collagen, as well as indirectly increased autotaxin levels.
“We found that these cells could regulate themselves by increased autotaxin production, which was being further enhanced by an autocrine loop,” Lama says. “What’s so fascinating about this is that it means the cell no longer needs an inflammatory environment, or stimulation in its environment, to produce the collagen. That’s extremely novel because we have never thought of these cells as essentially cancer cell-like in nature, but they are regulating their own behavior like a cancer cell does.”
She adds, “The dysregulated behavior of these cells essentially makes them become autonomous in behavior and helps us further understand why we can’t stop the scarring process just by changing the environment around the cell, which does not make a difference. They have already begun not listening to anything around them.”
Lama explains that this finding led the team to investigate new therapies.
“If we interrupt this pathway, we could potentially stop further development of lung scarring and save the graft,” she says.
Building on these findings, Lama and team examined two new therapeutic treatments for their potential in interrupting the pathway.
One treatment, PF-8380, targeted the enzyme, while the other treatment, AM095, targeted the receptor for lysophosphatidic acid.
Using a novel mouse lung transplant model of chronic rejection their laboratory developed, they were able to test if the drugs would decrease the scarring process.
Lama and team found that the mouse models treated with these orally administered drugs were protected from the scarring process of chronic rejection with significantly less fibrosis noted in their transplanted lungs.
The team hopes that these findings will lay the foundation for future clinical trials.
“Drugs targeting this pathway, such as autotaxin inhibitors and LPA1 receptor antagonists, have already been developed and are in clinical trials for other fibrotic conditions of the lung, such as idiopathic pulmonary fibrosis,” Lama explains. “Now we hope that we can consider similar therapies in BOS, a disease where we have no therapeutic options.”
Lama also explains that these findings should encourage the transplant community in general to consider anti-fibrotic treatments in patients with chronically rejected lungs, instead of just immune suppressive drugs that were given in the past.
“These findings suggest that understanding the pathways that activate a mesenchymal cell and targeting them is crucial if we want to contain the progression of BOS,” Lama says. “We hope this work, which started from the bedside when we examined the lavage fluid from our lung transplant recipients, will be able to be translated back from the bench to the bedside to make an impact on the lives of our patients.”




