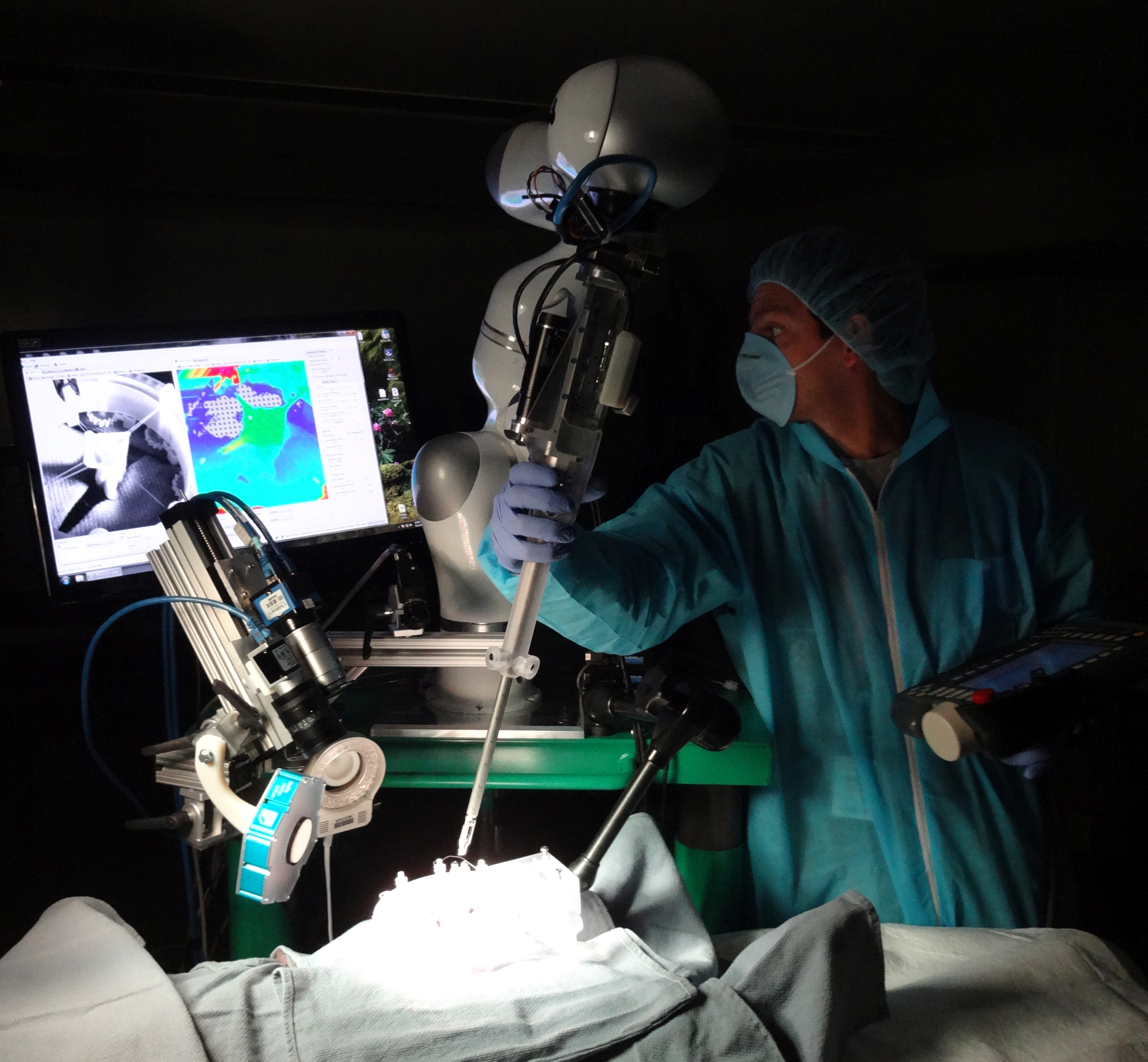
Surgeons and scientists from Sheikh Zayed Institute for Pediatric Surgical Innovation at Children’s National Health System are the first to demonstrate that supervised, autonomous robotic soft tissue surgery on a live subject (in vivo) in an open surgical setting is feasible and outperforms standard clinical techniques in a dynamic clinical environment.
The study, published today in Science Translational Medicine, reports the results of soft tissue surgeries conducted on both inanimate porcine tissue and living pigs using proprietary robotic surgical technology, Smart Tissue Autonomous Robot (STAR), developed at Children’s National. This technology removes the surgeon’s hands from the procedure, instead utilizing the surgeon as supervisor, with soft tissue suturing autonomously planned and performed by the STAR robotic system.
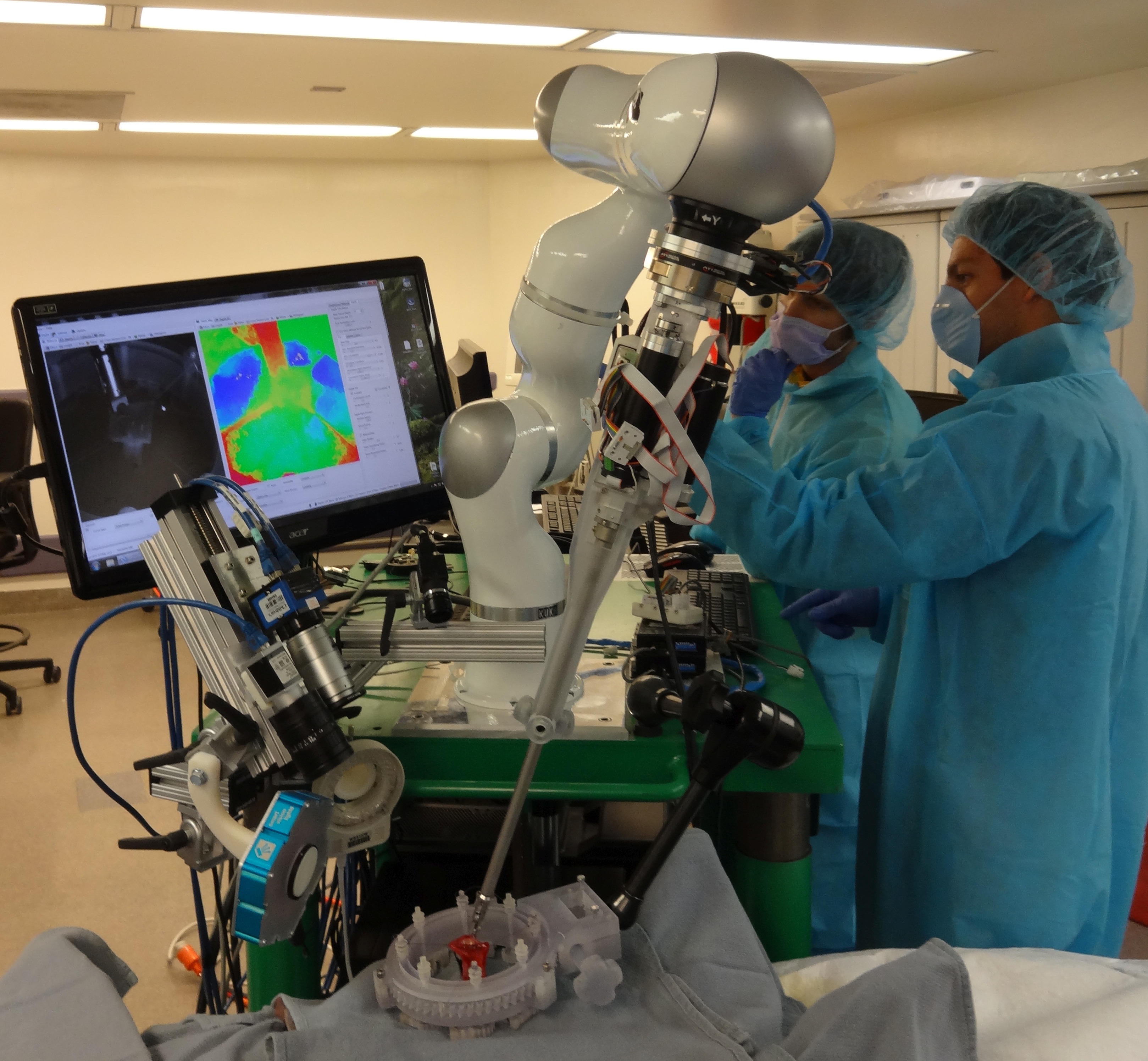
(All images credit: Sheikh Zayed Institute at Children’s National Health System)
Soft tissues are the tissues that connect, support or surround other structures and organs of the body such as tendons, ligaments, fascia, skin, fibrous tissues, fat, synovial membranes, muscles, nerves and blood vessels. Currently more than 44.5 million soft tissue surgeries are performed in the U.S. each year.
“Our results demonstrate the potential for autonomous robots to improve the efficacy, consistency, functional outcome and accessibility of surgical techniques,” said Dr. Peter C. Kim, vice president and associate surgeon in chief, Sheikh Zayed Institute for Pediatric Surgical Innovation. “The intent of this demonstration is not to replace surgeons, but to expand human capacity and capability through enhanced vision, dexterity and complementary machine intelligence for improved surgical outcomes.”
While robot-assisted surgery (RAS) has increased in adoption in healthcare settings, the execution of soft tissue surgery has remained entirely manual, largely because the unpredictable, elastic and plastic changes in soft tissues that occur during surgery, requiring the surgeon to make constant adjustments.
To overcome this challenge, STAR uses a tracking system that integrates near infrared florescent (NIRF) markers and 3D plenoptic vision, which captures light field information to provide images of a scene in three dimensions. This system enables accurate, uninhibited tracking of tissue motion and change throughout the surgical procedure. This tracking is combined with another STAR innovation, an intelligent algorithm that guides the surgical plan and autonomously makes adjustments to the plan in real time as tissue moves and other changes occur. The STAR system also employs force sensing, submillimeter positioning and actuated surgical tools. It has a bed-side lightweight robot arm extended with an articulated laparoscopic suturing tool for a combined eight degrees-of-freedom robot.
“Until now, autonomous robot surgery has been limited to applications with rigid anatomy, such as bone cutting, because they are more predictable,” said Axel Krieger, PhD, and technical lead for Smart Tools at Sheikh Zayed Institute for Pediatric Surgical Innovation at Children’s National. “By using novel tissue tracking and applied force measurement, coupled with suture automation software, our robotic system can detect arbitrary tissue motions in real time and automatically adjust.”
To compare the effectiveness of STAR to other available surgical procedures, the study included two different surgeries performed on inanimate porcine tissue (ex vivo), linear suturing and an end-to-end intestinal anastomosis, which involves connecting the tubular loops of the intestine. The results of each surgery were compared with the same surgical procedure conducted manually by an experienced surgeon, by laparoscopy, and by RAS with the daVinci Surgical System.
Intestinal anastomosis was the surgical procedure conducted on the living subjects (in vivo) in the study. The Children’s National research team conducted four anastomosis surgeries on living pigs using STAR technology and all subjects survived with no complications. The study compared these results to the same procedure conducted manually by an experienced surgeon using standard surgical tools.
“We chose the complex task of anastomosis as proof of concept because this soft tissue surgery is performed over one million times in the U.S. annually,” said Dr. Kim.
All surgeries were compared based on the metrics of anastomosis including the consistency of suturing based on average suture spacing, the pressure at which the anastomosis leaked, the number of mistakes that required removing the needle from the tissue, completion time and lumen reduction, which measures any constriction in the size of the tubular opening.
The comparison showed that supervised autonomous robotic procedures using STAR proved superior to surgery performed by experienced surgeons and RAS techniques, whether on static porcine tissues or on living specimens, in areas such as consistent suture spacing, which helps to promote healing, and in withstanding higher leak pressures, as leakage can be a significant complication from anastomosis surgery. Mistakes requiring needle removal were minimal and lumen reduction for the STAR surgeries was within the acceptable range.
In the comparison using living subjects, the manual control surgery took less time, eight minutes versus 35 minutes for the fastest STAR procedure, however researchers noted that the duration of the STAR surgery was comparable to the average for clinical laparoscopic anastomosis, which ranges from 30 minutes to 90 minutes, depending on complexity of the procedure.
Kim said that since supervised, autonomous robotic surgery for soft tissue procedures has been proven effective, a next step in the development cycle would be further miniaturization of tools and improved sensors to allow for wider use of the STAR system.
He added that, with the right partner, some or all of the technology can be brought into the clinical space and bedside within the next two years.




