A pathology test that applies artificial intelligence (AI) to characterize tissue samples can accurately predict clinically significant prostate cancer disease progression following surgery, according to a study conducted at the Icahn School of Medicine at Mount Sinai and published in Nature Prostate Cancer and Prostatic Diseases. The Precise MD post-op test automates the Gleason score (a grading system that has been used since the 1960s to establish the prognosis for a prostate cancer) through the application of an algorithm that integrates image analysis with protein biomarkers. Precise MD is a pathology platform that uses artificial intelligence and complex algorithms to translate data into clinical knowledge.
According to the American Cancer Society, prostate cancer is the second leading cause of cancer death in American men, behind lung cancer. Surgery is a treatment option that generally yields a good prognosis, but 25 to 30 percent of men who have surgery will have a recurrence. Accurate risk stratification post-surgery is essential to identifying patients at intermediate to high risk for clinically significant disease progression. Those patients could benefit from more attentive monitoring and possibly additional therapy, such as radiation or chemotherapy.
Researchers at the Center for Computational and Systems Pathology at Mount Sinai used AI-guided machine learning techniques to analyze cancer tissue samples from 590 patients who underwent a radical prostatectomy, an operation to remove the prostate gland and the tissues surrounding it. The Precise MD platform relies on cutting-edge microscopy with multispectral immunofluorescence to analyze cancer tissue architecture and biomarkers, enabling pathologists to see what the human eye cannot. Its analysis uses mathematical features to define tumor aggressiveness.
The Precise MD post-op test predicted significant disease progression with a greater degree of accuracy as compared with models that incorporated only clinical features such as the traditional Gleason score, or a Prostate-Specific Antigen (PSA) test; PSA is a substance produced by the prostate gland and elevated levels may indicate prostate cancer. Importantly, the Precise Post-op test reclassified 58 percent of intermediate risk patients as low risk and 42 percent as high risk for significant disease progression. Men identified as high risk by the Precise Post-op test may be appropriate candidates for additional monitoring and treatments, including chemotherapy and radiation.
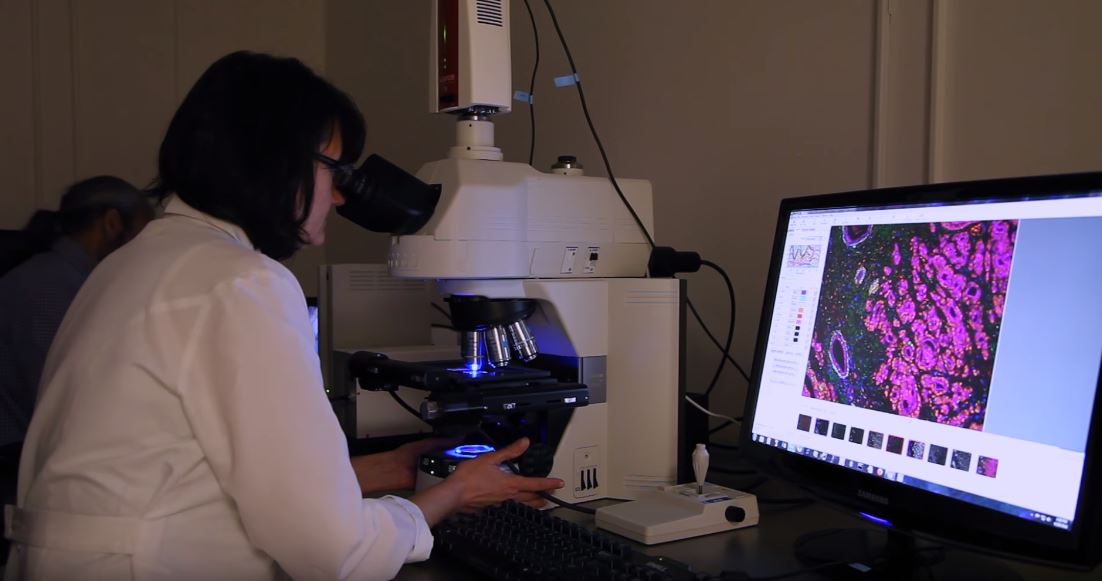
(Image search: screengrab from Mt Sinai Health System video)
“By refining diagnoses, we can guide patients toward the best treatment option and optimize care,” says senior author Carlos Cordon-Cardo, MD, PhD, Chair of the Department of Pathology at the Mount Sinai Health System and Professor of Pathology, Genetics and Genomic Sciences, and Oncological Sciences at the Icahn School of Medicine.
“The ability to generate more quantitative, less subjective, and enhanced cancer-grading systems will bring precision medicine to the practicing pathologist and provide treating physicians and their patients important information for guiding management decisions,” says lead author Michael Donovan, MD, PhD, Research Professor of Pathology at the Icahn School of Medicine at Mount Sinai.
“The opportunity to provide a more objective and comprehensive understanding of prostate cancer Gleason grading is especially important as our patients come from all over the world where practice patterns and expertise are often quite variable,” says Ash Tewari, MBBS, MCh, Chair of the Department of Urology at the Mount Sinai Health System and the Kyung Hyun Kim, MD Professor of Urology at the Icahn School of Medicine. “A test that improves risk discrimination, specifically for durable response to adjuvant androgen therapy, represents a significant step towards providing a comprehensive integrated patient-focused care path. We are currently using the Precise Post-Op test for our intermediate and high risk patients to better understand the available parameters of risk assignment in the postsurgical setting where appropriate management planning is oftentimes challenging.”
“Precision medicine is an innovative model of health care, and Mount Sinai is well positioned to provide our patients with more accurate diagnosis and tailored treatments,” says Dennis S. Charney, MD, Anne and Joel Ehrenkranz Dean, Icahn School of Medicine at Mount Sinai, and President for Academic Affairs, Mount Sinai Health System. “Machine learning systems in prostate cancer grading provide a more objective measure of risk assessment.”
The Henry Ford Hospital in Detroit and the Roswell Park Comprehensive Cancer Center in Buffalo, New York, provided patient samples for the study. Researchers say the Precise MD platform could be used to characterize any number of disease states, including but not limited to breast, melanoma, lung, and colon cancers as well as chronic inflammatory conditions such as inflammatory bowel disease.
“The introduction of machine learning systems in traditional prostate cancer grading represents an important step towards a more objective and biological reflection of personalized risk assignment,” says Howard Soule, PhD, Executive Vice President and Chief Scientific Officer of the Prostate Cancer Foundation.




