There was a time when most orthopedic surgeries were guaranteed to put a patient in the hospital for an extended period of time, enduring an intricate recovery process. That has changed, especially in recent years, as such a procedure is increasingly likely to take place in an ambulatory surgical center (ASC), with the patient heading home the same day.
According to Scott Zellner, the DePuy Synthes senior director of U.S. joint reconstruction marketing, the emergence of ASCs represents a key opportunity, especially as emerging payment models and tightening facility budgets demand innovation.
“We have found that as we are looking at redesigning patient care, it’s easier to do it in a bit of a green field, when you’re starting from the beginning, by leveraging an end-to-end approach that starts with understanding the customer need, from the implant to capabilities,” Zellner says. “You’re bringing together a new team, from the administrator to the surgeon, who are all focused on the patient and improving outcomes, the patient experience, and the overall cost of care. It can be more difficult to do that in an existing arena.”

(Image credit: Vail Valley Surgery Center)
Zellner notes that efficiency of care is a major factor, citing digital templating efforts on the part of DePuy Synthes that are specific to each patient. This helps cut down on the number of supplies loaded onto the prep cart ahead of a procedure. The practice doesn’t only have the potential to save money, it better suits smaller facilities.
“That’s important because most ASCs don’t have the central supply and the sterilization capacity to process seven to ten trays,” Zellner says, noting the team is often able to reduce the outlay to no more than a couple of trays instead.
The team approach undertaken by DePuy Synthes, as part of the Johnson & Johnson Medical Devices Companies, even extends to patient communication.
“When you’re in an ASC, the team literally has hours instead of days to work with the patient as they recover,” explains Zellner. “And so there is a heightened need for great patient outreach, education, and engagement in advance of that surgery. And not just with the patient, but with their caregivers.”
As part of the extended process, DePuy Synthes offers a capability called Digital Care Navigation, a data collection and analysis tool from CareSense provided by MedTrak. The program both collects data from the patient and guides them through the experience.
“For instance, when a patient is having a clinic visit, while they’re in the waiting room for 10 minutes, they’ll be given an iPad and they’ll answer 10 to 15 questions, depending on where they are in the journey,” Zellner says. “It’s customized to their situation, on how are they doing, and what concerns they may have.”
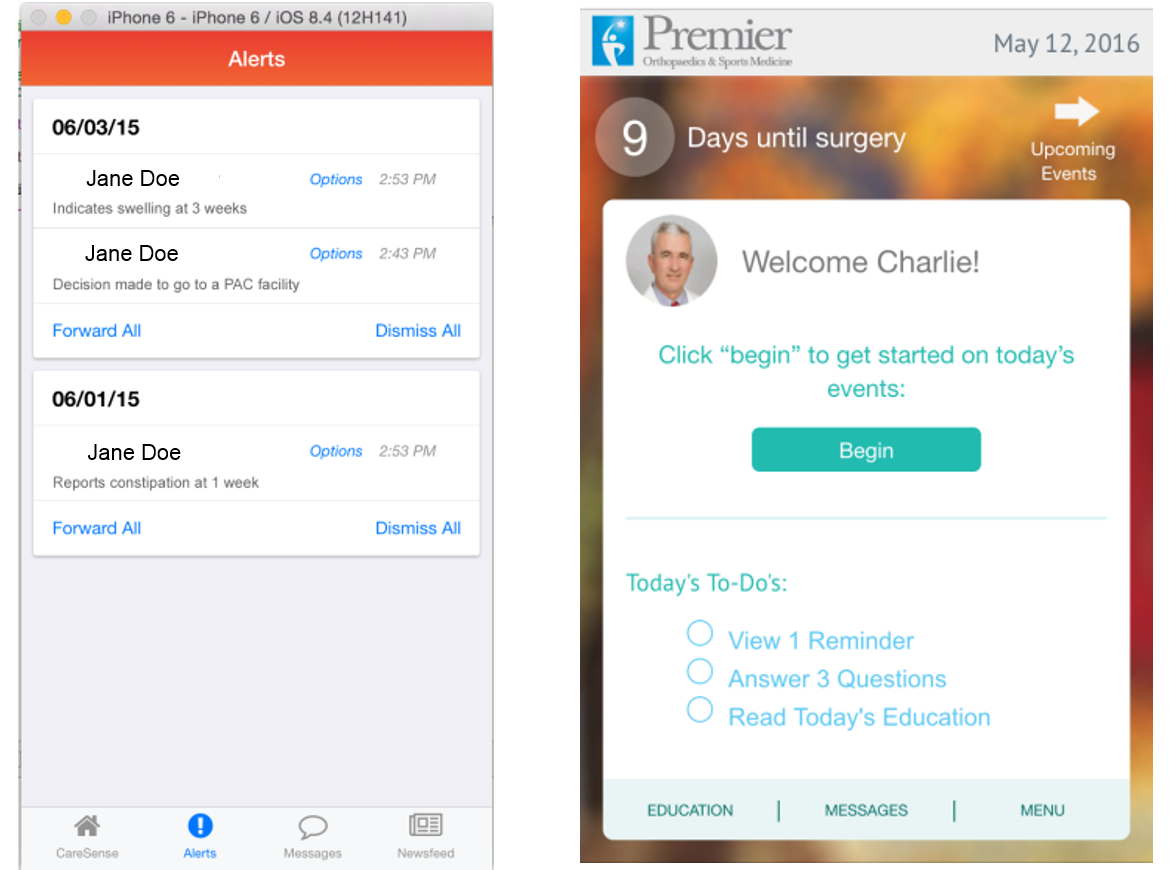
The Digital Care Navigation tool in Medtrak’s CareSense offers different interfaces for patients and physicians.
The information provided by the patient allows facilities to make certain the patient is staying on target and is completely satisfied with the experience, lessening the possibility that a negative development within 90 days of the procedure will compromise the bundled payment.
The program also gives patients a clearer pathway than what they can discern from the mountain of guidance healthcare facilities might feel obligated to provide.
“The problem is it’s pretty hard for a patient to find what they’re supposed to do any given day because it’s buried somewhere in 70 pages of instructions,” Zellner says. “What our Digital Care Navigation capabilities will do is provide the right information to the patient at the right time. If the patient needs to know, for instance, that day three pre-op they need to stop taking aspirin, a text or email or even a video can be provided to the patient at that point. So compliance goes way up, patients feel better because they know they’re doing the right thing at the right time, and nothing gets lost in a 70-page booklet.”
DePuy Synthes’ parent company, Johnson & Johnson, also developed Health Partner for Knees and Hips, a new science-based, tech-driven solution to help patients throughout the healthcare experience and enable them to take a proactive role in their health and well-being. Health Partner is focused on select health issues across the patient journey, including those that involve surgery as a potential option, and will bring to market three initial offerings — knee health and knee replacement, hip health and hip replacement, and patients considering bariatric surgery.
An unexpected result of the data digging undertaken with the Health Partner software is a shift in understanding about patient goals surrounding joint replacement surgeries. The easy assumption is that the patient motivation is always to alleviate pain. That remains basically accurate, but it’s not quite so simple.
“The program asks the patient, ‘What do you want to be able to do 90 days post-op?’” Zellner says. “You get great stories like, ‘I want to walk down the aisle with my daughter for her wedding,’ or, ‘I want to be able to bend down and hug my grandchildren.’ You get all sorts of inspirational stories about the functional, passionate, purposeful reasons why patients want to have knee replacement. They’re looking at knee replacement as a way to get their life back.”
Developing a more personalized understanding of what drives the patients to surgery is valuable. Leveraging the accumulated data into a more specific understanding of patient need is even more useful.
Despite perceptions that hospitals and ASCs will be locked in fierce competition for people with ailing knees, smartly studying the amassing information can instead help physicians make certain that patients wind up in the right place.
“In the future, we’ll be able to look at all the data that we’ve collected and understand which patients are — based on data and evidence — best suited for an inpatient procedure versus an outpatient procedure, which patients are going to need more monitoring versus others, which patients might need this education program versus that education program,” Zellner notes.
“The interesting thing about orthopedics is that we have been collecting survivorship data for decades now. Those knee replacements last 15, 20, 30 years. Now that we’ve moved to value-based healthcare, the question is: ‘Is my patient going to have a great outcome and be happy 90 days post-op?’ Healthcare providers are just now starting to collect, analyze, and use that data to make better decisions in determining the best care and therapy that should be provided to patients.”
This article originally appeared in the January/February 2017 issue of Surgical Products.




