Research scientist JeongHun Park. [Image courtesy of Georgia Tech]
Engineers in Scott Hollister’s lab are 3D-printing personalized airway support devices made from a biocompatible polyester. This material — called polycaprolactone (PCL) — already has approval from the FDA. Researchers use selective laser sintering to heat powdered polyester and bind it together.
According to Georgia Tech, PCL has the disadvantage of relatively stiff and linear mechanical properties. Because of this, its applications have yet to reach some critical biomedical needs like soft tissue engineering.
However, Jeong Hun Park, a research scientist in Hollister’s lab, led a team that successfully applied PCL to soft tissue engineering. The secret? Park says “3D auxetic design.” Auxetic materials, when stretched longitudinally, expand in the lateral direction. This differs from most materials that get thinner laterally.
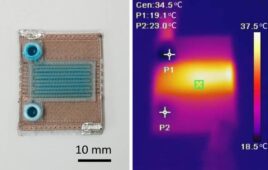
Because of this two-way expansion, these materials could change as human bodies change in size, shape, texture and density. The Georgia Tech team designed 3D-printed structures from tiny struts arranged at right angles. Its cube-shaped structures tested the design’s flexibility, strength and permeability.
“Although the mechanical properties and behavior of the 3D structure depend on the inherent properties of the base material — in this case, PCL — it can also be significantly tuned through internal architecture design,” Park said in a post on the Georgia Tech website.
More about the auxetic material
The researchers describe the material as a network structure designed by assembling unit cells. These cells have struts and intersecting joints and the rotation of those joints under compression or extension can lead to the two-way expansion. It also enables advanced performance for a printed device, the team says.
Features include impact energy absorption, indentation resistance and high flexibility. According to Hollister, the new structure registers about 300 times more flexible than typical solid PCL structures that come out of the lab.
Combining flexibility and strength is crucial, according to Park, because the ultimate goal is to apply the structure to develop a breast reconstruction implant. The team hopes to develop an implant with comparable biomechanical properties to native breast tissue. Park says a biodegradable breast implant option currently doesn’t exist in the clinical setting.
These implants serve as a scaffold, park says, eventually degrading before the body absorbs the material. It still maintains similar mechanical properties to native breast tissue, though.
“We expect that native tissue will be first infiltrated into the pores of the biodegradable implant,” Park said. “Tissue volume will then increase within the implant as it degrades and eventually the device itself is replaced with the tissue after complete degradation of the implant.”
What comes next for the 3D printing method?
The researchers hope their 3D-printed breast implant eventually offers reconstructive support while facilitating the growth of new tissue. The space between the struts could make the difference for a larger device, making it softer and more pliable. Hydrogels that foster cell and tissue growth could eventually fill those spaces, too, they said.
Park’s team also designed inner voids and spaces inside the struts, creating a microporosity that enables the mass transport of oxygen, nutrients, and metabolites to nurture the expansion and growth of a cellular network.
Park and Emory surgeon Angela Cheng have work underway to submit a grant for further research and testing. In the meantime, the team has plans to adapt the technology for other applications. One collaborator, Mike Davis, has a lab at Emory focused on cardiac regeneration. Hollister says the new material could help to reconstruct infarcted or necrotic myocardial tissue.
Additionally, Park developed an auxetic version of the pediatric tracheal splint.
“The advantage there is, with this design, it can expand in two directions,” Park said. “So, as young patients grow, the new device will grow with them.”