[Image from Wyss Institute]
Researchers are using organs-on-chips more frequently to study human organs and tissues. They offer a better approach to testing drugs because they can mimic blood flow, mechanical microenvironment and how different tissues are able to physically interface with each other in specific organs. It can take weeks for the human cells to grow into intact differentiated and functional tissues on chips.
The Harvard Wyss Institute for Biologically Inspired Engineering wanted to non-invasively monitor the health and maturity of cells and the electrical functions of normally electrically active cells in the organs-on-chips over a long period of time.
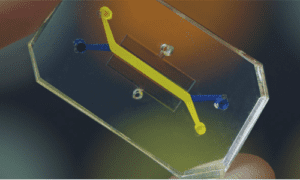
The team, led by Donald Ingber and in collaboration with Wyss Core Faculty member Kit Parker, fit organs-on-chips with embedded electrodes that could accurately and continuously monitor trans-epithelial electrical resistance (TEER), which is used to measure the tissue health, differentiation and electrical activity of living cells.
“These electrically active organ chips help to open a window into how living human cells and tissues function within an organ context, without having to enter the human body or even remove the cells from our chips,” Ingber, who is the Wyss Institute’s founding director, said in a press release. “We can now start to study how different tissue barriers are wounded in real time by infection, radiation, drug exposure or even malnutrition, and how and when they heal in response to new regenerative therapeutics.”
TEER measurements help quantify the flow of ions between electrodes and across a tissue-tissue interface that is made of organ-specific epithelium and endothelium. The epithelial cells form tissue layers that cover the inner surfaces of most internal organs and endothelial cells line adjacent blood-transporting vessels and capillaries. Both cell layers are a barrier to small molecules and ions that protect organs and allow for a specialized function. Drug toxicities, infections, inflammation and other injurious stimuli disrupt the barriers, so TEER measurements can be used to assess baseline functional integrity of the cell layers and damage responses that are created by drugs or other toxic agents.
“Using a new layer-by-layer fabrication process, we created a microfluidic environment in which TEER-measuring electrodes are integral components of the chip architecture and are positioned as close as possible to the tissues grown in one or both of two parallel running channels,” said Olivier Henry, Wyss Institute staff engineer. “In contrast to past electrode designs, this fixed geometry allows accurate measurements that are fully comparable within and between experiments, and that tells us exactly how tissues like that of lung or gut mature within a channel, keep in shape and break down under the influence of drugs or other manipulations.”
With a TEER measurement chip that was integrated with multielectrode arrays, the researchers were able to build a beating, vascularized heart chip that had human cardiomyocytes cultured within one microfluidic channel and separated by a thin semi-permeable membrane from an endothelium-lined vascular channel. The researchers then tested the technology and treated the vascularized heart chip with an inflammatory stimulant that they knew would disrupt endothelial barriers or a heart stimulant that acts on cardiomyocytes.
“This new chip enables us to perform live electrophysiological measurements to assess the integrity of the endothelial barrier in the heart using TEER measurements, while simultaneously quantifying the beating frequency of the heart cells using MEA,” said Ben Maos, a technology development fellow at the Wyss Institute and one of the study’s authors. “This allows us to reveal how drugs affect heart functions in a scenario where the two cell populations are closely coupled.”
Harvard researchers recently used organs-on-chips to recreate kidney functions on a chip using human stem cells. Organ-on-chips are still a fairly new concept and the FDA is testing the technology behind them.
The research was published in Lab on a Chip and was funded by the Wyss Institute and the Defense Advanced Research Projects Agency.
“The future of organs-on-chips is instrumented chips: the idea that the experimenter is taken out of the loop during data collection. Continuous data collection off of organ mimics is what we need to measure efficacy and safety of drugs during long-duration experiments. These kinds of technologies offer us a granularity we have not had before,” Parker said.
[Want to stay more on top of MDO content? Subscribe to our weekly e-newsletter.]








